Introduction
Facial paralysis has many causes, and the etiology determines the likelihood of spontaneous return of function, as in most cases of idiopathic facial paralysis (Bell palsy). The transected or severely damaged nerve requires repair in order to achieve a satisfactory return of function. The problem remains a frustrating one because residual weakness and synkinesis is an inevitable component of the healing process. Nonetheless, most patients benefit greatly from modern techniques of repair.
History of the Procedure
The history of nerve repair dates back to Galen, who discussed the possibility of nerve regeneration in 200 AD. Paul of Arginia performed the first documented suture repair in 600 AD. The work of Waller in the 1850s was crucial to the understanding of peripheral nerve degeneration and regeneration. By the 1930s, Balance and Duel were reporting their results with facial nerve grafting. Lathrop and Myers advanced these techniques during World War II. In 1970, Scaramella described the technique of cross-face nerve grafting, further modified by Anderl.
Today, repair of the facial nerve involves several choices of procedures. These include direct repair, cable nerve grafting, and nerve crossover techniques. Facial nerve decompression for cases of intact but damaged nerves and procedures of facial reanimation distinct from the repair of the facial nerve are discussed elsewhere in this journal (see Dynamic Reanimation for Facial Paralysis).
Problem
Paralysis of the facial nerve is a cause of significant functional and aesthetic compromise. Functional concerns primarily involve adequate protection of the eye, with a real risk of exposure keratitis if not properly addressed. In addition, swallowing, drooling, and speech difficulties may arise. The degree of suffering these patients feel, however, is often far greater than these functional problems alone would produce. Patients with facial paralysis, especially younger ones, may experience tremendous psychosocial distress about their condition. Poor self-image and difficulty interacting with peers and family members can be devastating.
Repair of the facial nerve is generally a concern in cases of permanent complete facial paralysis. This may involve all or selected branches of the facial nerve. Frustration arises in the difficulty often found in achieving an excellent result. Synkinesis and hypofunction are an expected result, and these problems are among the challenges to be overcome with future improved techniques.
Etiology
The causes of facial paralysis are many. They may be divided into congenital, neoplastic, traumatic, inflammatory, and idiopathic.
Congenital facial paralysis, such as in the well-described although poorly understood Möbius syndrome, is uncommon.
Idiopathic facial paralysis (Bell palsy) makes up the most common type. These cases are often thought to be the result of virally induced inflammation of the nerve resulting in compromise of function, swelling, and vascular compromise. Facial nerve repair is uncommonly required because most of these patients regain function spontaneously. When paralysis is permanent, some advocate facial nerve decompression in selected cases. This article focuses on cases requiring various nerve grafting techniques, rather than procedures of decompression.
Traumatic injuries, which include blunt and penetrating trauma, as well as iatrogenic injury during surgery, comprise the next most common category. The site of injury to the facial nerve may be intracranial, intratemporal, or external to the stylomastoid foramen. Acoustic neuroma surgery is an example of a disease process and procedure that puts the facial nerve at risk, in this case in the cerebellopontine angle. Any of these sites of injury may be amenable to techniques of facial nerve repair, with the exception of injuries near the root entry zone of the nerve, in which case the length of facial nerve stump available to repair may be inadequate.
Neoplastic causes of facial paralysis commonly involve tumors of the parotid gland, typically malignant. Facial nerve schwannomas, acoustic neuromas, and neoplasms of the brain are among the less common causes of facial paralysis. Inflammatory and infectious causes of facial paralysis can occur. Infectious agents implicated include virally mediated conditions such as herpes zoster (eg, Ramsey Hunt syndrome), mumps, Coxsackie virus, and mononucleosis. Bacterial infections include sequelae of otitis media and Lyme disease.
Inflammatory conditions include sarcoidosis.
Pathophysiology
The facial nerve undergoes degeneration of the distal segment after significant injury, as described by Waller. Sunderland classified the degree of injury into 5 types. These 5 degrees describe the pathophysiologic events associated with each of the disorders described above that may affect the nerve.
First-degree injury is referred to as neurapraxia, in which a physiologic block is produced by increased intraneural pressure. An example is by external compression. The covering layers of the nerve (ie, endoneurium, perineurium, epineurium) are not disrupted, and the nerve is capable of stimulation. Full return of function without synkinesis is observed.
Second-degree injury involves a similar mechanism, but the compression is unrelieved and results in degeneration of the nerve axons. This is termed axonotmesis, and again, excellent return is expected, although recovery may take several months. Nerve stimulation is compromised, so distinguishing this from axonotmesis is difficult. Degrees 3 through 5 involve loss of endoneural, perineural, and epineural tubes, respectively. Fourth- and fifth-degree injuries imply partial or complete transection of the nerve. Regeneration is incomplete, and synkinesis is inevitable. Repair of the facial nerve is generally performed in cases of complete paralysis.
Presentation
History reveals the cause of the facial paralysis and is extremely important in treatment planning. The signs and symptoms of facial paralysis are obvious. The House-Brackman grading scale for facial paralysis is used to objectively describe the degree of paresis or paralysis. Patients demonstrate a lack of tone in addition to no movement on the affected side.
Of particular importance is the inability to adequately protect the eye. This should be assessed by careful inspection for signs of exposure keratitis, ability to close the eye, and the presence or absence of a Bell phenomenon. Questioning of partners and family members can reveal the adequacy of eye closure during sleep. Measures to protect the eye (eg, lubricants, artificial tears, eye taping at night) must be instituted as appropriate.
Indications
Facial nerve repair is an option for facial paralysis without a reasonable likelihood of spontaneous return of function. Essential in determining whether repair is indicated are the cause of the paralysis and the duration of time since the injury. Some general principles are helpful. In general, transected nerves produce the best result when reapproximated. This produces an intact motor nerve supply from the facial motor nucleus in the pons to the muscle endpoint and is preferable whenever possible. If direct repair without tension is possible, this is performed. Otherwise, a cable graft may be inserted to produce a tensionless coaptation of the proximal nerve stump to the distal branch or branches. Nerve crossover techniques are used when the proximal nerve stump is inadequate or inaccessible, preventing its use for grafting.
Another simple rule of thumb is that the sooner one can repair an injured facial nerve, the better the long-term result. This has in the past been somewhat controversial, but it is now believed to be true for most cases. In cases of trauma, in which the continuity of the nerve is in question, exploring within the first 3 days after injury is extremely desirable. This is because of the ability of the surgeon within this timeframe to use a nerve stimulator intraoperatively to identify the branches of the facial nerve. Once degeneration has occurred, stimulation of the nerve is not possible, and identifying the branches in an inflamed field can be extremely difficult.
Fibrosis of the nerve, fibrosis of the motor endplate, and atrophy of the muscle all ensue after injury. The surgeon is in a race against this inevitable process. Thus, the likelihood of success in a repair performed 18 months after the onset of paralysis is sure to be compromised, in comparison with the result obtained with repair in the first month after injury.
Waiting may be appropriate in specific instances, depending on the health of the patient, oncologic surveillance issues, and other concerns. Nonetheless, when possible, maximizing the patients' chance of a satisfactory outcome is desirable. Consider alternatives to repair, such as facial reanimation procedures, in such a case. In addition, patient-specific factors influence the clinical decision-making. In an elderly patient, slower nerve regeneration is expected, with a likely poorer result than in a younger patient. If the patient's life expectancy is short, for example, one may choose an adjunctive procedure to produce an immediate improvement, such as a dynamic muscle sling, rather than a nerve repair that takes quite some time to accomplish in the best of circumstances.
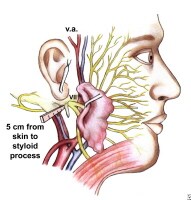
Relevant Anatomy
The facial nerve may be divided into intracranial, intratemporal, and extratemporal components. The intracranial portion of the facial nerve may be considered to include the supranuclear component (ie, voluntary motor cortex, internal capsule, extrapyramidal system, midbrain, pons) and the facial nerve nucleus and intracranial facial nerve. The intratemporal portion begins as the nerve enters the internal acoustic meatus and includes the well-described meatal, labyrinthine, tympanic, and vertical segments. The nerve then exits the stylomastoid foramen and soon divides at the pes anserinus. The subsequent branching to the temporal, zygomatic, buccal, marginal mandibular, and cervical branches shows some variability from person to person.
The blood supply to the facial nerve begins with the middle cerebral artery supplying the motor cortex. The facial nucleus in the pons is supplied by the anterior inferior cerebellar artery and the short and long circumferential arteries. The facial nerve proper is then supplied by the anterior inferior cerebellar artery, the middle meningeal artery, and the stylomastoid branch of the postauricular artery. These tend to overlap; however, the region just proximal to the geniculate ganglion is thought to be somewhat susceptible to vascular compromise secondary to the poorer redundancy present there compared with other areas.
Some discussion of the microanatomy is warranted for the purposes of this topic. Approximately 7000 neuron cell bodies make up the facial nerve, each of which innervates approximately 25 muscle fibers. The axons are surrounded by myelin, produced by the Schwann cells surrounding the axons. Three membranes comprise the nerve sheath. The epineurium is the outer covering, composed of loose areolar tissue, which separates the fascicles and holds them together. The perineurium is the next more inner layer. This is a dense layer of cells that are metabolically active and function as a diffusion barrier. The perineurium provides considerable strength to the nerve sheath. The individual nerve fibers are then each surrounded by endoneurium.
The spatial orientation of the nerve has traditionally been a matter of some debate. In the cortex and brainstem, the nerve is spatially oriented. If it continued in an organized spatial orientation through its extra-axial course, this would have implications for the facial nerve surgeon's technique of repair and ability to help to some degree to prevent synkinesis. It would also allow some identification of the area of injury of the nerve based on clinical findings. Although such clinical observations have been made by several authors, the evidence suggests that the spatial orientation is not present in the extra-axial facial nerve.1
For further information, please see the eMedicine article Facial Nerve Anatomy.
Contraindications
Repair of the facial nerve is contraindicated when the motor endplate muscle unit is no longer functional. This occurs after long-standing paralysis in which fibrosis occurs along with atrophy of the facial musculature. In such instances, reinnervation is not successful. The motor endplate muscle unit may fuse in cases of long-standing paralysis (ie, >1-1.5 y). Electrophysiologic testing can help to determine this.
Age of the patient is considered by some to be a relative contraindication. Anecdotal evidence demonstrates poorer results of reinnervation techniques in elderly patients. The nerve regenerates more slowly, and results are ultimately poorer than in procedures performed on younger patients.
Planned radiation therapy is not a contraindication to facial nerve repair. Regeneration of nerve function has been demonstrated despite subsequent ablative doses of radiation.
Facial nerve repair may be contraindicated in other situations. These would include instances when the general health status of the patient prevents elective surgery.
More on Facial Nerve Repair |
 Overview: Facial Nerve Repair Overview: Facial Nerve Repair |
| Workup: Facial Nerve Repair |
| Treatment: Facial Nerve Repair |
| Follow-up: Facial Nerve Repair |
| Multimedia: Facial Nerve Repair |
| References |


I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóa