Introduction
The zygomaticomaxillary complex (ZMC) plays a key role in the structure, function, and aesthetic appearance of the facial skeleton. It provides normal cheek contour and separates the orbital contents from the temporal fossa and the maxillary sinus. It also has a role in vision and mastication. The ZMC provides lateral globe support necessary for binocular vision. The zygomatic arch is the insertion site for the masseter muscle and protects the temporalis muscle and the coronoid process.
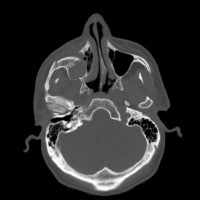
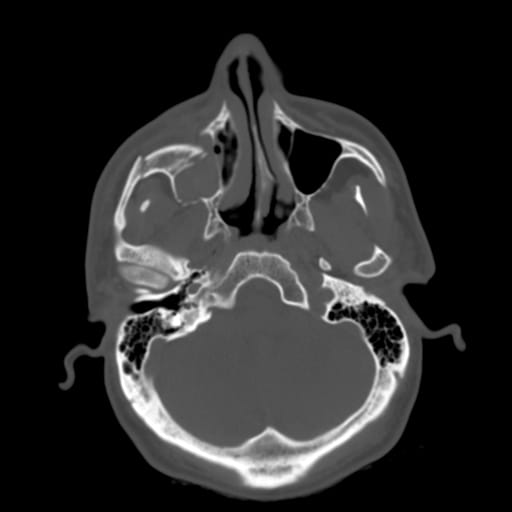
The frequency of ZMC fractures is second only to nasal fractures, which are the most common type of facial fracture.1 The prominent convex shape of the zygoma makes it vulnerable to traumatic injury, as seen in the image below. Even minimally displaced ZMC fractures can result in functional and aesthetic deformities. Successful repair of ZMC fractures requires an accurate diagnosis, appropriate surgical exposure, and precise reduction to reconstitute the complex 3-dimensional anatomy.
For excellent patient education resources, visit eMedicine's Back, Ribs, Neck, and Head Center, Breaks, Fractures, and Dislocations Center, and Eye and Vision Center. Also, see eMedicine's patient education articles Broken Jaw, Facial Fracture, and Black Eye.
Problem
See Clinical.
Frequency
A much higher percentage of zygomaticomaxillary complex (ZMC) fractures occur in males (80%) than in females (20%). Incidence of ZMC fractures peaks in persons aged 20-30 years. Women who have been domestically abused are more likely to suffer ZMC fractures and orbital blow-out fractures,2 while mandible fractures are more common when the female victim did not know the assailant.
Etiology
The most common causes of zygomaticomaxillary complex (ZMC) fractures include personal altercations, falls, motor vehicle accidents, and sports injuries. Other associated facial fractures occur in 25% of patients who sustain ZMC fractures.3
Pathophysiology
See Relevant Anatomy for a discussion of the impact of zygomaticomaxillary complex (ZMC) fractures on other facial structures.
Classification
Many authors have devised classification schemes for zygomaticomaxillary complex (ZMC) fractures.3,4,5 Zingg (1992) separates these injuries into types A, B, and C.6 Type A injuries are isolated to one component of the tetrapod structure, including the zygomatic arch (type A1), the lateral orbital wall (type A2), and the inferior orbital rim (type A3). Type B fractures involve all 4 buttresses (ie, classic tetrapod fracture). Type C injuries are complex fractures with comminution of the zygomatic bone itself. These classification schemes are of little clinical significance; however, they are helpful in research and physician communication.
Type A fractures are relatively uncommon. Type B and C fractures account for 62% of ZMC injuries.3 Types B and C fractures most commonly occur at the zygomaticomaxillary and zygomaticotemporal buttresses. The zygomaticofrontal buttress is the strongest of the 4 ZMC buttresses. Significant disruption at this site usually implies a high velocity injury with comminution in other areas. The weakest bone of the ZMC complex is the orbital floor. Type A3, B, and C injuries result in orbital floor disruption, which places the orbital contents at risk.
Presentation
The initial evaluation of facial trauma patients is focused on areas that can result in the greatest morbidity. Airway control and hemodynamic stability are the primary concerns. Next, spinal cord injury must be ruled out by a thorough clinical and/or radiological examination.
Finally, any overt globe injury should be evaluated. After the patient has been stabilized, a thorough history can be taken and physical examination can be performed. A complete head and neck examination will reveal most bony or soft tissue injuries. When zygomaticomaxillary complex (ZMC) fractures are identified, an ophthalmologic consultation should be obtained.
The most common symptoms associated with ZMC fractures include pain, edema, and ecchymosis of the cheek and eyelids. Malar flattening and palpable periorbital step-offs, often occur. The traumatic force and pull of the masseter muscle may result in medial, inferior, and posterior rotation of the zygoma.7 Trismus (ie, reduced jaw mobility) may result from compression of the zygomatic arch on the temporalis muscle and coronoid process. Orbital floor disruption can result in subcutaneous emphysema. Infraorbital nerve injury may result in anesthesia or paresthesias of the cheek, nose, upper lip, and lower eyelid.
Jelks (1987) reported a 14-40% incidence of significant intraocular injury in patients with ZMC fractures that involved the orbital floor.8 For this reason, preoperative ophthalmology consultation is essential in patients with orbital floor injuries. Disruption of the bony orbit often results in expansion of the orbital volume and herniation of orbital contents. Inferior (hypophthalmos) and posterior (enophthalmos) globe displacement both occur.
Extraocular muscle contusion or entrapment may result in diplopia. Upward gaze diplopia is most common, secondary to entrapment of the inferior rectus muscle and soft tissue surrounding it. However, any of the extraocular muscles may be involved. Comparing forced-duction tests on each eye can help to identify the specific site of muscle entrapment. This study is much easier to perform under general anesthesia. Evaluation of unanesthetized patients is often difficult because of poor patient cooperation.
Compression of the orbital contents occurs less frequently. These injuries result in decreased orbital volume and displacement of the globe both superiorly (hyperophthalmos) and anteriorly (exophthalmos). These injuries are associated with an increased risk of optic nerve injury and visual loss. Physical findings such as severe conjunctival hemorrhage or hyphema are suggestive of direct globe injury, rupture, and visual loss.
Indications
Surgical intervention is indicated in patients with injuries that result in a significant cosmetic or functional deformity, such as the following:
- Visual compromise: Significant exophthalmos and orbital apex syndrome are indications for emergent surgical decompression.
- Extraocular muscle dysfunction: Muscle contusion, local tissue edema, or extraocular muscle entrapment and strangulation can cause extraocular muscle dysfunction. Edema and contusion usually resolve without long-term sequelae; however, muscle entrapment does not resolve. Muscle necrosis with long-term diplopia can occur if entrapped muscle is not released expediently.
- Globe displacement: Enophthalmos or hypophthalmos following acute injury becomes more pronounced with resolution of edema. Acute orbital dystopia requires surgical intervention.
- Significant orbital floor disruption: Large orbital floor fractures result in long-term enophthalmos and hypophthalmos. The definition of a "significant orbital floor injury" varies among authors. However, injuries encompassing 25-50% of the orbital floor have a higher risk of long-term enophthalmos. In these patients, orbital exploration with surgical repair should be considered.
- Displaced or comminuted fractures: These injuries generally result in cosmetic deformity and require surgical repair.
Relevant Anatomy
The malar eminence is the most prominent portion of the zygomaticomaxillary complex (ZMC) and is located approximately 2 cm inferior to the lateral canthus. The malar eminence corresponds to the central portion of the ZMC. From this central position, 4 bony attachments to the skull are evident, namely, a superior attachment to the frontal bone (frontozygomatic suture line), a medial attachment to the maxilla (zygomaticomaxillary suture line), a lateral attachment to the temporal bone (zygomaticotemporal suture line), and a deep attachment to the greater wing of the sphenoid bone (zygomaticosphenoidal suture line).9 Some authors describe the zygomaticomaxillary and zygomaticosphenoidal suture lines as a single unit. Using this definition, ZMC fractures are called tripod fractures. However, the term tetrapod fracture is a more accurate description because 4 suture lines are disrupted.
The term ZMC fracture describes a spectrum of injuries that includes nondisplaced fractures, fractures displaced at an isolated buttress, and severely comminuted fractures with bone loss. Information about the degree and severity of the overall injury can be extrapolated from the location of the fractures.
The frontozygomatic and zygomaticosphenoidal buttresses are very strong. Isolated injuries in these areas are uncommon. When displaced fractures are noted, a high velocity injury with other associated fractures is likely.
The inferior orbital rim is a common location for displaced and comminuted fractures. These injuries can be isolated, but they are often associated with orbital floor fractures. The zygomaticomaxillary buttress is commonly disrupted and associated with V2 paresthesias. Isolated injuries often occur in the zygomatic arch because of its length and unprotected location.
Contraindications
Contraindications to surgical repair of zygomaticomaxillary complex (ZMC) fractures include medical instability and globe injuries. Orbital exploration in the presence of a hyphema or ruptured globe can result in exacerbation of the injury.

I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóa