Introduction
Surgery in the upper third of the face, whether reconstructive or cosmetic, can be considered to involve at least 1 of 3 regions: the central forehead, the hair-bearing scalp, and the temporal regions. Anatomy must be reviewed in the context of the eyebrow-forehead-temple continuum.
Surface Anatomy
The forehead constitutes the upper third of the face. It is delineated superiorly by the hairline and inferiorly by the glabella and frontonasal groove centrally and the eyebrows overlying the supraorbital ridges laterally. The hairline is not a stable landmark among individuals; factors of sex, age, familial characteristics, and the influences of culture and fashion decide the hairline position for individuals. Although the hairline defines the anatomic boundary between the forehead and the scalp, consideration must be given to anticipated patterns of baldness in the future because scars may be exposed with a receding hairline.
The density of eyebrow hair generally remains stable with age, although it may frequently be altered in appearance by plucking or tattooing. Eyebrow position, contour, and movement are important features of facial expression. The medial eyebrow hairs are almost vertical in orientation, while laterally they become more horizontal. The eyebrow forms an arc laterally, with the peak at the junction of the medial two thirds and the lateral third. The brow is straighter and thicker in males, being at the level of the superior orbital rim; it is more arched, thinner, and higher in females.
The superior orbital margin forms a well-marked prominence that may be palpated along its length. It frequently presents the supraorbital notch, which can be felt at the junction of the medial third and lateral two thirds. The Latin root of the word glabella means hairless and smooth, and the glabella is such in youth; however, glabellar transverse and vertical rhytides are common with age. Superiorly, between the eyebrows and the hairline, smoothness gives way to horizontal forehead rhytides with age. Rhytides may be considered to give an opportunity for scar camouflage in surgery.
The curved arc of the temporal line is palpable at the lateral limits of the forehead and is made more apparent with the action of the temporalis muscle with mastication. The superficial temporal artery is generally palpable in the temple, which is important in the consideration of a temporal artery biopsy and when local vascularized flaps are planned. The lateral orbital margin is visible and palpable in its extent, and the frontozygomatic suture frequently may be felt as a small depression some 10 mm superior to the lateral canthus. The superior margin of the zygomatic arch is generally palpable, extending between the lateral orbital rim and the anterior border of the tragus.
The course of the frontal branch of the facial nerve passes through the temple and forehead, placing this nerve at risk of injury at the time of surgical dissection. The usual trajectory of the nerve is from a point 5 mm below the tragus to a point 15 mm above the lateral extremity of the brow. Over the zygomatic arch, it is situated halfway between the lateral canthus and the inferior helix. This places it about 2.5 cm lateral to the lateral canthus.
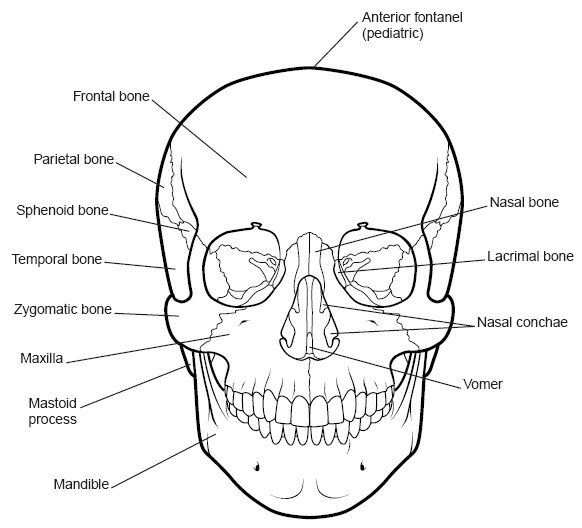
Bones of the Forehead
The bones of the forehead form the scaffold on which the soft tissues are draped. The frontal bone presents an anterior surface that is convex anteriorly. It articulates with (1) the parietal bones posteriorly at the coronal suture, (2) the nasal bones and the frontal process of the maxilla anteriorly and medially, (3) the frontal process of the zygoma at the frontozygomatic suture laterally, and (4) within the temporal fossa, with the greater wing of the sphenoid. The frontal bone also presents an orbital surface and an intracranial surface that is not discussed in this article.
The superciliary ridges are prominences of the frontal bone above the orbital margins that meet in the midline in the glabella. They are significantly more prominent in males. The superior orbital rim presents a supraorbital notch or foramen through which courses the supraorbital neurovascular bundle. Bilateral notches are present in 49% of skulls, bilateral foramina in 26%, and one notch and one foramen in 25%.
The temporal crest runs from the zygomatic process of the frontal bone superiorly and posteriorly to become continuous with the temporal line on the parietal bone.
The mean calvarial thickness is 6.8 to 7.7 mm, which can be safely drilled to a depth of 3-4 mm. The bone is thicker in the female than the male, and the thickest is in the parietal bone behind the coronal suture; the superotemporal site is thinnest, with a thickness between 4.71 and 6.14 mm. Drilling in the midline is to be avoided, keeping in mind the location of the sagittal sinus.
The Forehead and Scalp
The scalp is traditionally considered in 5 layers: skin, subcutaneous tissue, galea aponeurotica, loose areolar tissue, and periosteum. These layers continue into the forehead, where, in the region of the eyebrow, galea gives way to the muscles of facial expression.
Skin
The forehead skin is the thickest facial skin and is rich in sebaceous glands and sweat glands.
Subcutaneous tissue
Richly vascularized, subcutaneous tissue contains a homogenous layer of adipose tissue. Numerous transverse fibrous septa from the frontalis muscle to the dermis are found within this layer in the forehead. These septa are partially responsible for the deep transverse forehead rhytides.
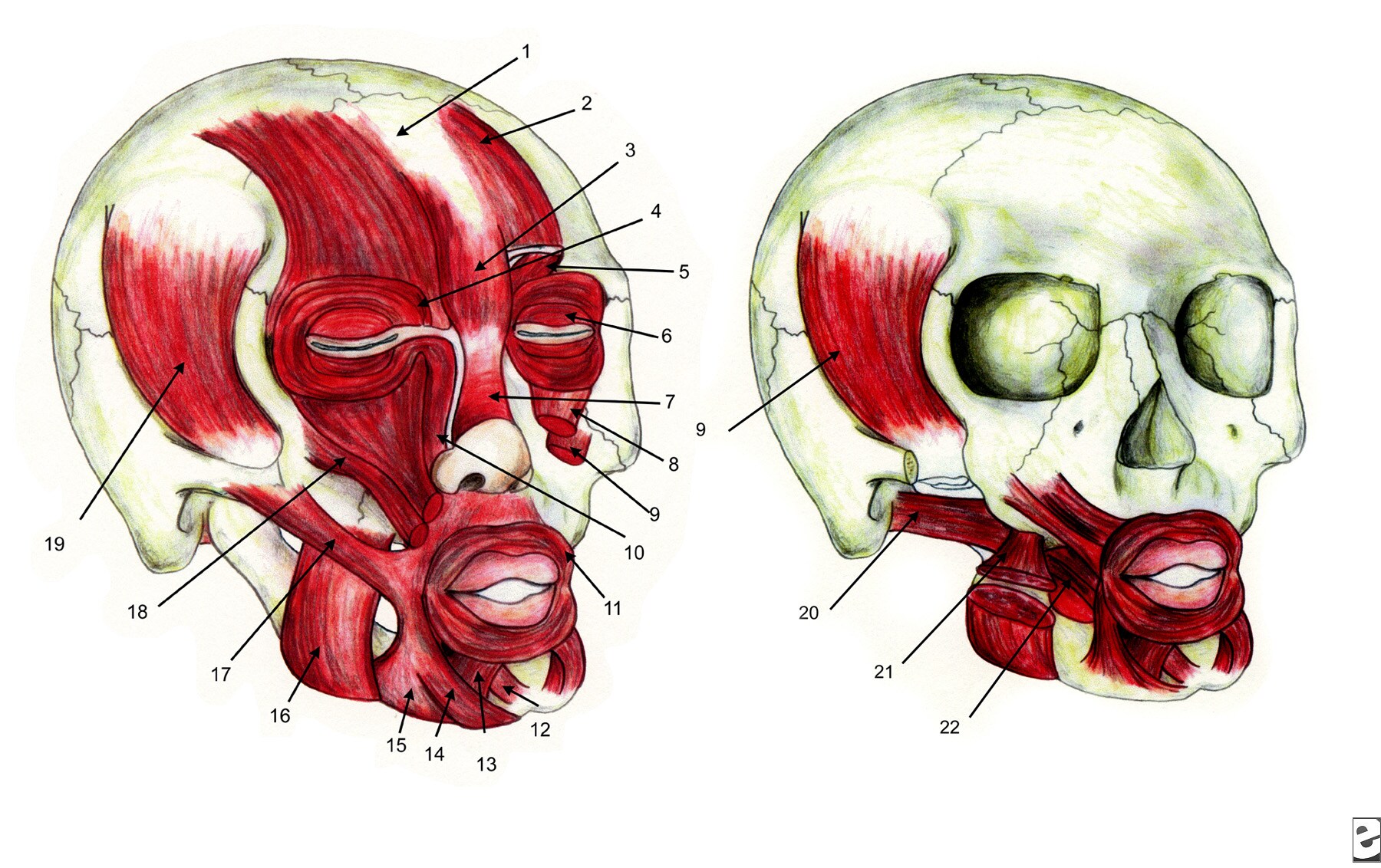
Muscles and Aponeurosis of the Forehead
The muscular layer of the eyebrow is below the subcutaneous tissue. This layer is composed of the elevator muscle (frontalis) and the depressor muscles (procerus, corrugator supercilii, orbital portion of the orbicularis oculi).
Frontalis muscle
The paired frontalis muscles are the primary elevators of the brow. The vertically orientated muscle fibers offer no true bony insertion but blend with the brow depressor muscles, which do have bony insertions (the procerus medially, the corrugator and orbicularis oculi centrally, the orbicularis oculi laterally). Deep to the frontalis muscle, a potential space that allows movement of the frontalis over the periosteum is found. The frontalis also has multiple attachments to the dermis of the forehead skin, causing transverse forehead creases.
Innervation is by the frontal branch of the facial nerve.
The frontalis is continued posteriorly by the large thin epicranial aponeurosis (galea aponeurotica). The galea aponeurotica encloses the frontalis muscle with a thin superficial layer over the muscle and a deeper well-defined layer beneath the muscle. This deeper layer is firmly attached to the supraorbital margin, contributing to the arcus marginalis. Laterally, the galea conceptually continues as the superficial temporal fascia (STF). Posteriorly, the galea continues as the occipitalis muscle. The 2 bellies of the occipitalis take their origin from the periosteum and bone of the superior nuchal line of the mastoid portion of the temporal bone and insert into the galea aponeurotica. Innervation is by the posterior auricular branch of the facial nerve.
Corrugator superciliaris muscle
The paired corrugator superciliaris muscles arise from the frontal bone near the superomedial orbital rim, anteriorly and slightly cephalad to the trochlea. The muscle runs superolaterally through the fibers of orbicularis oculi and frontalis before inserting into the medial eyebrow skin. The corrugator muscle is a brow depressor, pulling the brow medially and inferiorly, producing vertical glabellar folds. Innervation is from terminal branches of the frontal branch of the facial nerve.
Procerus muscle
The flat, thin procerus muscle takes origin from the nasal bone and inserts into the glabella and lower mid forehead. It lies between the paired frontalis muscles. The procerus is a brow depressor, forming horizontal nasal root creases.
Orbicularis oculi muscle
The orbicularis oculi muscle should be considered a muscle of the eyelid rather than of the brow; however, the orbital portion extends in a wide circular fashion around the orbit, interdigitating with other muscles of facial expression of the brow. It has a curved origin from the medial orbital margin, being attached to the superomedial orbital margin, maxillary process of the frontal bone, the medial palpebral ligament, the frontal process of the maxilla, and the inferomedial orbital margin. Fibers from the medial origin sweep around the orbital margin in a horseshoe fashion. The muscle fibers extend superiorly to intermix with the frontalis and corrugator supercilii muscles and laterally to cover the STF.
Functionally, the orbital portion of the muscle is used in forced eyelid closure and, hence, acts as a brow depressor. The superomedial portion of each orbicularis muscle is also referred to as the depressor supercilii muscle. Innervation is from branches of the facial nerve. The nerves are horizontally orientated and innervate the muscle from the undersurface.
Anatomic dissection reveals a distinct layer of fibroadipose tissue posterior to the orbicularis oculi and frontalis muscles, termed the retroorbicularis oculi fat (ROOF). ROOF is analogous to the suborbicularis oculi fat (SOOF) of the lower eyelid. The ROOF frequently continues inferiorly over the superior orbital rim to overlie the orbital septum. The function of this tissue may be to enhance eyebrow mobility.
Loose Areolar Tissue
The subgaleal space is used as a plane of dissection in forehead surgery. Connective tissue lies between the galea and the periosteum, which can be easily divided with a semisharp dissector. At the supraorbital margin, the space is traversed by the supraorbital and supratrochlear neurovascular bundles.
The subgaleal vascular plane receives blood supply peripherally from all the major scalp vessels and is a source for blood supply to both galea aponeurotica and periosteum. Subgaleal dissection for a forehead lift may remove one source of blood supply to a raised forehead flap. Subperiosteal dissection raises the subgaleal tissue with the forehead flap and preserves this source of blood supply.
Pericranium
The pericranium lies adherent to the bone but can be readily elevated to give a relatively avascular subperiosteal space, suitable for the optical cavity required in endoscopic browlifting. Anteriorly, the pericranium continues into the orbit as the periorbita. Along the supraorbital rim, the periosteum fuses with the orbital septum at the arcus marginalis.
Sullivan et (2006) have shown the presence of 3 retaining ligaments, the inferomedial (12 mm lateral to the midline at the superior orbital rim), the superomedial (13 mm lateral to midline and 10 mm above the superior orbital rim), and the superotemporal (23 mm lateral to midline and 10 mm above the rim).1Supraorbital and Supratrochlear Nerves
Sensory innervation of the forehead and anterior scalp is supplied by the supraorbital and supratrochlear nerves, being branches of the ophthalmic division of the trigeminal nerve.
The supraorbital nerve and vessels emerge from the supraorbital foramen or notch and continue superiorly. Near this exit, the supraorbital nerve trunk divides into a deep and a superficial branch. The deep branch courses superolaterally, running parallel and 0.5 to 1.5 cm medial to the superior temporal line of the skull in the loose areolar tissue between the galea and the pericranium. The terminal branches of this deep supraorbital nerve branch pierce the galea near the coronal suture to supply scalp sensation to the fronto-parietal region. The superficial division lies medially at its origin and quickly divides into multiple branches that pierce the frontalis muscle. These smaller branches pass cephalad to supply the forehead and up to 3.5 cm of the frontal scalp. The supraorbital nerve also supplies the upper eyelid sensation by small eyelid branches.
Supratrochlear nerves exit the orbit at the superior orbital rim through a notch, above the trochlea and medial to the supraorbital notch. Most skulls (97%) possess bilateral supratrochlear notches; however, 1% possess bilateral foramina, and 2% have a notch on one side and a foramen on the other. At the supraorbital rim, the nerves penetrate the corrugator muscle and the frontalis muscle toward the skin and may be damaged here during corrugator resection. The nerves supply cutaneous sensation to a central vertical strip of forehead and to the medial upper eyelid.
The Temporal Region
The tissue layers in the temporal region are the skin, subcutaneous fat, superficial temporal fascia (STF), deep temporal fascia (DTF), and temporal muscle. A problem in the discussion of anatomy in this region is the variable nomenclature used for the various fascial layers and fat pads.
For the surgeon, important features in the temple region include the frontal branch of the facial nerve and the superficial temporal artery.
The skin and subcutaneous tissues continue from the scalp and forehead, with a variable degree of hair-bearing skin in the temples.
The STF represents the continuance of the superficial musculoaponeurotic system (SMAS) of the face and the galea aponeurotica system of the scalp. This multilaminated fascial layer is loosely adherent to the subdermal fat and is intimately associated with the frontal branch of the facial nerve and the superficial temporal vessels. It is also called the temporoparietal fascia.
A loose areolar plane, termed the subaponeurotic plane, separates the STF from the DTF and is the plane of dissection commonly used when operating in the temporal region. It allows dissection directly on the surface of the DTF. This plane is relatively avascular, but 2-3 perforating veins are frequently sentinels to the approaching zygomatic arch. The one (or sometimes two) sentinel vein present lateral to the orbital rim bears a fairly constant relationship to the bony landmarks. The temporal division of the facial nerve is usually found cephalad to the sentinel vein.
The DTF is a thick, dense connective tissue layer overlying the temporalis muscle. It has a firm attachment to the superior temporal line. Several centimeters above the zygomatic arch, the DTF splits into a superficial layer and a deep layer. The superficial layer of the DTF attaches to the superficial superior margin of the zygomatic arch. The deep layer of the DTF attaches to the deep superior margin of the zygomatic arch. Enveloped between the 2 layers of the DTF lies the superficial temporal fat pad. This vascular adipose deposit is supplied by the middle temporal artery. Deep to the deep layer of the DTF lies the deep temporal fat pad, which represents a superior extension of the buccal fat pad. This extension passes superiorly deep to the zygomatic arch, to lie between the deep layer of the DTF and the temporalis muscle proper.
Along the anterior limits of the superior temporal line, the STF and the galea aponeurotica fuse with the DTF and the central forehead periosteum to form a conjoint fascia. Dissection of the fascial layers in this region requires sharp dissection.
Superficial temporal artery
The superficial temporal artery is a terminal branch of the external carotid artery. Its origin lies within the parotid gland, and it ascends to cross the zygomatic arch about 10 mm anterior to the tragus. Above the arch, the vessel is invested within the STF. The superficial temporal artery gives numerous terminal branches, including the transverse facial, the middle temporal, the parietal, and the frontal branches.
Frontal branch of the facial nerve
The frontal branch of the facial nerve supplies motor innervation to the muscles of facial expression of the eyebrows and forehead. It courses within the STF, traveling within its deep surface. The course of the nerve places it at risk of injury at the time of surgical dissection over the zygomatic arch and in the temple and forehead. Its usual trajectory is from a point 5 mm below the tragus to a point 15 mm above the lateral extremity of the brow. Over the zygomatic arch, it is found about 2.5 cm lateral to the lateral canthus, placing it halfway between the lateral canthus and the inferior helix.
Conclusions
An intimate knowledge of the functional anatomy of the forehead and eyebrows is required by the surgeon when dealing with reconstructive and cosmetic problems. Familiarity with neurovascular structures and fascial planes in the forehead and scalp and into the temporal region is required for optimal surgical outcomes.
Multimedia
 | Media file 2: Skull. |
Keywords
forehead anatomy, anatomy of the brow, central forehead, hair-bearing scalp, temple, central forehead

I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóa