Introduction
Background
Few emergencies pose as great a challenge as neck trauma. Because a multitude of organ systems (eg, airway, vascular, neurological, gastrointestinal) are compressed into a compact conduit, a single penetrating wound is capable of considerable harm. Furthermore, seemingly innocuous wounds may not manifest clear signs or symptoms, and potentially lethal injuries could be easily overlooked or discounted.
Airway occlusion and exsanguinating hemorrhage pose the most immediate risks to life. From the time when Ambroise Pare successfully treated a neck injury in 1552, debate has continued about the best approach for particular neck wounds. Awareness of the various presentations of neck injuries and the establishment of a well-conceived multidisciplinary plan prior to the traumatic event is critical for improving patient outcome.
Pathophysiology
A clear understanding of the anatomic relationships within the neck and the mechanisms of injury is critical to devising a rational diagnostic and therapeutic strategy.
Structures at risk
With the neck protected by the spine posteriorly, the head superiorly, and the chest inferiorly, the anterior and lateral regions are most exposed to injury. The larynx and trachea are situated anteriorly and are therefore readily exposed to harm. The spinal cord lies posteriorly, cushioned by the vertebral bodies, muscles, and ligaments. The esophagus and the major blood vessels are between the airway and spine.
Two fascial layers invest the neck: the superficial fascia (enveloping the platysma muscle) and the deep cervical fascia. The deep cervical fascia envelops the sternocleidomastoid and trapezius muscles as well as demarcates the pretracheal region (including the trachea, larynx, thyroid gland, and pericardium), the prevertebral area (containing the prevertebral muscles, phrenic nerve, brachial plexus, and axillary sheath), and the carotid sheath (enclosing the carotid artery, internal jugular vein, and vagus nerve).
Musculoskeletal structures at risk include the vertebral bodies; cervical muscles, tendons, and ligaments; clavicles; first and second ribs; and hyoid bone.
Neural structures at risk include the spinal cord, phrenic nerve, brachial plexus, recurrent laryngeal nerve, cranial nerves (specifically IX-XII), and stellate ganglion.
Vascular structures at risk include the carotid (common, internal, external) and vertebral arteries and the vertebral, brachiocephalic, and jugular (internal and external) veins.
Visceral structures at risk include the thoracic duct, esophagus and pharynx, and larynx and trachea.
Glandular structures at risk include the thyroid, parathyroid, submandibular, and parotid glands.
Associated structures at risk of intrathoracic injuries include the esophagus, tracheobronchial tree, lung, heart, and great vessels.
Anatomic zones
Dividing the neck into anatomic zones or regions assists in the evaluation of injury. Serving as the line of demarcation, the sternocleidomastoid separates the neck into anterior and posterior triangles. Most of the important vascular and visceral organs lie within the anterior triangle bounded by the sternocleidomastoid posteriorly, the midline anteriorly, and the mandible superiorly. Except for individual nerves to specific muscles, few vital structures cross the posterior triangle, which is delineated by the sternocleidomastoid, the trapezius, and the clavicle (with the exception of the region just superior to the clavicle).
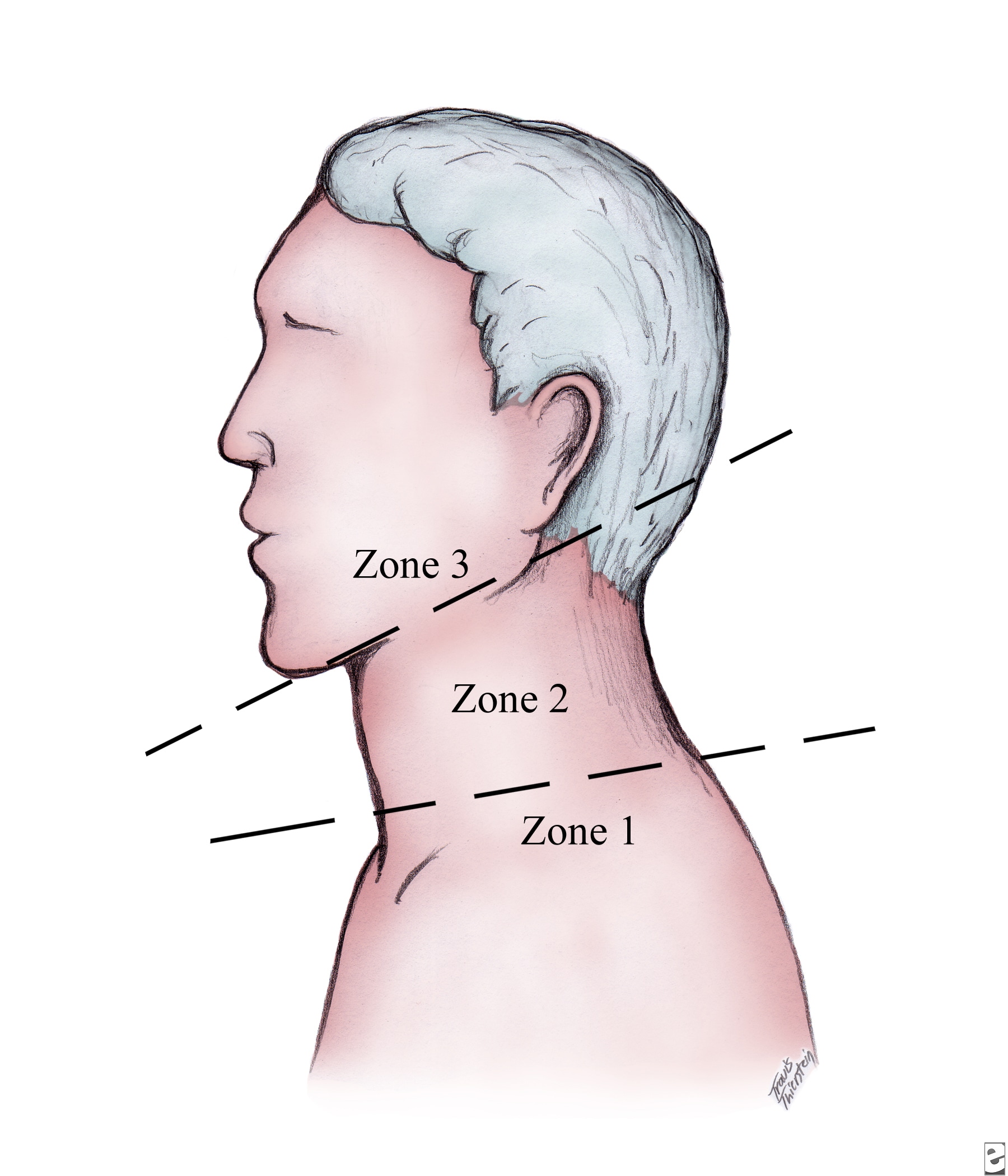
For clinical purposes, the neck is partitioned into 3 zones (as is shown in the image below).
Zone I (as is illustrated in the image below), the base of the neck, is demarcated by the thoracic inlet inferiorly and the cricoid cartilage superiorly.
Structures at greatest risk in this zone are the great vessels (subclavian vessels, brachiocephalic veins, common carotid arteries, aortic arch, and jugular veins, trachea, esophagus, lung apices, cervical spine, spinal cord, and cervical nerve roots. Signs of a significant injury in the zone I region may be hidden from inspection of the chest or the mediastinum.
Zone II (as is illustrated in the image below) encompasses the midportion of the neck and the region from the cricoid cartilage to the angle of the mandible.
Important structures in this region include the carotid and vertebral arteries, jugular veins, pharynx, larynx, trachea, esophagus, and cervical spine and spinal cord. Zone II injuries are likely to be the most apparent on inspection and tend not to be occult. Additionally, most carotid artery injuries are associated with zone II injuries.
Zone III (as is seen in the image below) characterizes the superior aspect of the neck and is bounded by the angle of the mandible and the base of the skull.
Diverse structures, such as the salivary and parotid glands, esophagus, trachea, vertebral bodies, carotid arteries, jugular veins, and major nerves (including cranial nerves IX-XII), traverse this zone. Injuries in zone III can prove difficult to access surgically.
Penetrating trauma
More than 95% of penetrating neck wounds result from guns and knives, with the remainder resulting from motor vehicle accidents, household injuries, industrial accidents, and sporting events. Generally, people experiencing a gun shot wound (GSW) sustain greater injury than those with stab wounds because of a bullet's proclivity to penetrate deeper and cause cavitation, thus damaging structures lying outside the tract of the missile.1
High-velocity bullet wounds (>2000-2500 ft/s) tend to follow a direct and predictable pathway, while low-velocity bullets travel a more erratic pathway, often demonstrating no direct relationship to the entrance or exit wounds. Additionally, high-velocity bullet wounds produced by military-style weapons or hunting rifles generate shock waves that devitalize surrounding tissues. High-velocity missiles and their ensuing blast effects may suck debris into the wound tract or cause secondary injuries from bullet or bone fragmentation. Low-velocity injuries may be produced by .22-caliber and .38-caliber handguns that have a muzzle speed of 300 ft/s to 800 ft/s. Furthermore, lower-energy injuries (knife, handgun, long-range birdshot or buckshot) cause a 50% lesser frequency of clinically significant injuries no matter what the zone of injury.
A lateral transcervical GSW is more likely to cause a grave injury than a GSW involving injury to only one side of the neck. Close-range GSWs of the neck that produce massive destruction are usually fatal. After a GSW to the neck, surgery is indicated in 75% of cases, whereas only 50% of neck stab wounds require surgical exploration.
Vascular injuries arising from penetrating trauma may occur directly, causing a partial or complete transection of the vessel or inducing formation of an intimal flap, arteriovenous fistula, or pseudoaneurysm. Injury to the blood vessels can also result from external compression or mural contusion. Thrombosis is the most common complication of blood vessel injury, occurring in 25-40% of patients.
The internal jugular vein (9%) and carotid artery (7%) are the most common sites of vascular injuries. Injury to the pharynx or the esophagus occurs in 5-15% of cases. The larynx or the trachea is injured in 4-12% of cases. Major nerve injury occurs in 3-8% of patients sustaining penetrating neck trauma. Spinal cord injury occurs infrequently and almost always results from direct injury rather than secondary osseous instability.
Blunt trauma
Blunt trauma to the neck typically results from motor vehicle crashes but also occurs with sports-related injuries (eg, clothesline tackle), strangulation, blows from the fists or feet, and excessive manipulation (ie, any manual operation such as chiropractic treatment or physical realignment or repositioning of the spine).
In motor vehicle crashes in which the driver is not belted, the driver is in danger of thrusting forward with the head extended, forcing the anterior neck against the steering column. Shoulder harnesses appear to offer some, though incomplete, protection against blunt neck trauma; cerebral vessel and laryngeal injuries secondary to shoulder strap compression have occurred.
Nonpenetrating trauma can injure a blood vessel through a multitude of mechanisms.
Direct forces can shear the vasculature. Excessive rotation and/or hyperextension of the cervical spine causes distention and stretching of the arteries and veins producing shearing damage and resultant thrombosis. Intraoral trauma may extend to the cerebral blood supply. Basilar skull fractures may disrupt the intrapetrous portion of the carotid artery. Impact to the exposed anterior aspect of the neck may crush the larynx or the trachea, particularly at the cricoid ring, and compress the esophagus against the posterior spinal column. A sudden increase in intratracheal pressure against a closed glottis (eg, improper wearing of a seat belt), a crush bruise (eg, clothesline tackle), or a rapid acceleration-deceleration action may cause a tracheal injury.
Strangulation may result from hanging (partial or complete suspension of the body from the neck), ligature suffocation, manual choking, and postural asphyxiation (eg, seen in children when the neck is placed over an object and the body weight produces compression). Significant cervical spine and spinal cord damage happens in only those hangings that involve a fall from a distance greater than the body height. Simple asphyxiation is not the major cause of death in hanging injuries. Cervical spinal disruption subsequent to strangulation is almost uniformly fatal.
Frequency
United States
Neck trauma accounts for 5-10% of all serious traumatic injuries. Approximately 3500 people die every year from neck trauma secondary to hanging, suicide, and accidents.
Mortality/Morbidity
During the Vietnam era, when mandatory exploration and vascular repair was the standard of care for penetrating neck wounds, the mortality rate for the civilian population was 4-7%. Today, the overall mortality rate has decreased to 2-6%.
Initially missed cervical injuries secondary to neck trauma result in a mortality rate of greater than 15%. Ten percent of neck wounds lead to respiratory compromise. Loss of the airway patency may occur precipitously, resulting in mortality rates as high as 33%.
Zone I injuries are associated with the highest morbidity and mortality rates.
Sex
Trauma is more common among males than among females.
Age
Most people who experience neck trauma are adolescents and young adults.
Clinical
History
Since many critical organs and structures remain at risk from neck trauma, clinical manifestations may vary greatly. The presence or absence of symptoms can be misleading, serving as a poor predictor of underlying damage. For example, only 10% of patients with blunt vascular damage develop symptoms in the first hour.
- Use all available sources when trying to establish the mechanism of injury. Question the patient, involved bystanders, and prehospital personnel. Clarify events surrounding the traumatic event, establish the amount of time that elapsed since the injury, and confirm the patient's baseline condition. Determine the amount of blood that was lost at the scene and whether the patient lost consciousness. Determine if any evidence of recent drug or alcohol ingestion is present.
- When neck trauma results from a motor vehicle crash, inquire about seat belt use, location of the patient in the car (driver or front or back seat passenger), deployment of an air bag, and magnitude of car damage (eg, intrusion, steering column and windshield intact or broken).
- In the event of a penetrating trauma, try to verify details about the weapon used, such as type and size of knife or type and caliber of gun.
- For patients with injuries due to hanging, try to determine the suspension time (when the patient was last seen), drop height, ligature used, history of alcohol or drug abuse, and history of suicide attempts.
- Characterize pain (eg, location, nature, intensity, onset, radiation), and document the nature and location of all stated injuries.
- Cardiovascular manifestations range from bleeding to symptoms normally associated with a cerebrovascular accident.
- Symptoms relating to the aerodigestive tract include dyspnea, hoarseness, dysphonia, and dysphagia.
- CNS problems include paresthesias, weakness, plegia, and paresis.
Physical
A standard approach to the patient with neck trauma is advised.
- The primary survey should consist of determination of airway patency, breathing, and adequacy of circulation. Keep in mind that loss of patency of the airway may occur precipitously. The patient should be fully exposed and any disabilities noted.
- On secondary survey, the neck should be methodically examined, searching for clues that indicate damage to vital contents. The sensitivity of the physical examination to identify all significant neck damage remains controversial. Some experts in the field of trauma assert that physical examination alone is sufficient to assess zone II for injury, while others believe that diagnostic testing is mandatory. The literature is not definitive.
- A single examination is not sufficient because the onset of signs of injury may be delayed and progressive with neck trauma.
Other general principles to follow are described below.
- Careful inspection the neck for a breach of the platysma. Invested by the most superficial fascia, violation of the platysma serves as a marker for possible serious penetrating neck wounds. Any violation of the platysmal muscle should be an alert to the potential for grave damage to the contents of the neck. If the platysma is violated, determine whether the wound lies anterior (anterior triangle) or posterior (posterior triangle) to the sternocleidomastoid muscle, and determine in what zone the injury is found. Try to specify the direction of the wound tract (eg, toward or away from the midline or clavicle). About 50% of cases of penetrating neck trauma in which the platysma is violated have no further injury. If the platysma is clearly not violated by a penetrating injury, the patient can be safely cleared of a significant underlying injury.
- Consider an arterial injury of the neck in patients manifesting any degree of gross bleeding or presence of a hematoma.
- Hard signs of an arterial injury include a large expanding hematoma, severe active or pulsatile bleeding, shock unresponsive to fluids, signs of cerebral infarction, presence of a bruit or thrill, and diminished distal pulses. Virtually all patients with hard signs of an arterial injury require operative repair.
- Soft signs, such as a nonexpanding hematoma and paresthesias, do not improve the predictive value of an arterial injury more than indicating the proximity of the wound to a major vessel.
- The presence of a pulse does not exclude a vascular injury, and absence of a pulse is not diagnostic of vascular damage.
- Clinical findings are lacking initially in almost one third of patients with an arterial injury of the neck.
- Nearly one third of carotid artery injuries are associated with a central neurological deficit.
- Unnecessary probing or manipulation of the wound or performing any action that may cause the patient to gag, choke, or cough is discouraged. Any of these reactions may dislodge a clot and provoke a life-threatening hemorrhage.
- Perforation of the pharynx or the esophagus following blunt neck trauma occurs infrequently (present in approximately 10% of trauma admissions). Initially, the patient may have no complaints, with the physical examination often failing to reveal any injury. Indirect signs of aerodigestive injuries include hematemesis, odynophagia, subcutaneous emphysema, and blood in the saliva or in the aspirate of a nasogastric tube. Because the esophagus lacks a serosa layer, it is more susceptible to iatrogenic injury such as following endoscopy, passage of a nasogastric tube, or inadvertent esophageal intubation. Esophageal perforation is the most serious and rapidly fatal trauma-induced perforation of the GI tract.
- Examine the patient who has been strangulated. Note location and depth of marks, petechial hemorrhages of the skin and subconjunctival tissue (Tardieu spots), noisy or impaired respiration or phonation (eg, stridor, hoarseness, poor air movement), and palpable crepitus or tenderness over the larynx and trachea. Check for neurological deficits.
Attention to specific signs that indicate injury to specific structures.
- Signs of spinal cord or brachial plexus injury
- Brachial plexus injuries sustained from blunt trauma tend to involve the upper nerve roots (C5-C7), diminishing the capacity of the upper arm while sparing strength and sensation of the lower arm. A radical avulsion of the brachial plexus results in a flaccid, numb extremity.
- Quadriplegia occurring with complete transection of the spinal cord manifests as an absence of all motor, sensory, and reflex function below the level of injury. Bilateral neurological findings imply a spinal cord injury until proven differently.
- Pathological reflexes, such as the Babinski reflex (extension of big toe) and Hoffmann sign (overactive muscle-stretch reflex), may be present.
- Brown-Séquard syndrome results from hemisection of the spinal cord, causing ipsilateral motor paralysis with contralateral sensory deficits.
- Priapism and loss of the bulbocavernous reflex may occur, and rectal tone may be poor.
- Urinary retention, fecal incontinence, and paralytic ileus can occur from spinal cord damage.
- Horner syndrome (ipsilateral miosis, enophthalmos, anhidrosis) results from disturbances of the stellate ganglion.
- Neurogenic shock is a diagnosis of exclusion and is characterized by persistent bradycardia despite hypotension.
- Hypoxia and hypoventilation can follow disruption of phrenic innervation to the diaphragm.
- Signs of larynx or trachea injury
- Voice alteration
- Hemoptysis
- Stridor
- Drooling
- Sucking, hissing, or air frothing or bubbling through the neck wound (It may be provoked by coughing.)
- Subcutaneous emphysema and/or crepitus
- Hoarseness
- Dyspnea
- Distortion of the normal anatomic appearance (eg, loss of normal landmarks, asymmetry, flattened thyroid prominence, tracheal deviation)
- Pain on palpation or with coughing or swallowing
- Pain with tongue movement implies injury to the epiglottis, hyoid bone, or laryngeal cartilage
- Crepitus (This hallmark sign of disruption to aerodigestive tract is noteworthy in only one third of cases.)
- Signs of penetrating injuries of the heart, aorta, and great vessels
- Hemorrhage, usually associated with large wounds (eg, gun shot wounds [GSWs])
- Massive hemothorax
- Hypotension
- Tamponade (if intrapericardial portion of aorta is injured)
- Weak or absent carotid or brachial pulse
- Paradoxical pulse (decrease in systolic BP with inspiration)
- Bruit
- Cervical or supraclavicular hematoma
- Bleeding from the entrance wound
- Upper extremity ischemia
- Coma
- Hemiparesis
- Respiratory distress secondary to tracheal compression
- Signs of tracheobronchial or lung injury
- Subcutaneous emphysema
- Cough
- Respiratory distress
- Hemoptysis, usually secondary to a disrupted bronchial artery
- Tension pneumothorax
- Continuous air leak persisting after chest tube insertion
- Mediastinal crunch (Hamman crunch)
- Intercostal retractions
- Decreased breath sounds
- Hyperresonance to percussion of the contralateral hemithorax, associated with hyperinflation of the unaffected lung
- Tachypnea
- Agitation
- Hypotension
- Tachycardia
- Hypoxia
- Shifting of the trachea and the apical heartbeat away from the injured side
- Signs of carotid artery injury
- Decreased level of consciousness
- Contralateral hemiparesis
- Hemorrhage
- Hematoma
- Dyspnea secondary to compression of the trachea
- Thrill
- Bruit
- Pulse deficit
- Signs of jugular vein injury
- Hematoma
- External hemorrhage
- Hypotension
- Signs of cranial nerve injuries
- Facial nerve (cranial nerve VII) - Drooping of the corner of the mouth
- Glossopharyngeal nerve (cranial nerve IX) - Dysphagia (altered gag reflex)
- Vagus nerve (cranial nerve X, recurrent laryngeal) - Hoarseness (weak voice)
- Spinal accessory nerve (cranial nerve XI) - Inability to shrug a shoulder and to laterally rotate the chin to the opposite shoulder
- Hypoglossal nerve (cranial nerve XII) - Deviation of the tongue with protrusion
- Thoracic duct injury: This is usually asymptomatic and tends to be an incidental finding during surgical exploration.
- Signs of esophagus and pharynx injury
- Dysphagia
- Bloody saliva
- Sucking neck wound
- Bloody nasogastric aspirate
- Pain and tenderness in the neck
- Resistance of neck with passive motion testing
- Crepitus
- Bleeding from the mouth or nasogastric tube
Causes
Neck trauma may be caused by penetrating or blunt trauma.
- Penetrating trauma
- GSWs
- Stab wounds
- Blunt trauma
- Motor vehicle crashes; ie, padded dash syndrome, whereby an unrestrained front seat occupant sustains injury to the anterior neck structures striking the steering column or dashboard
- Sports-related injuries and clothesline injuries, where the rider of a motorcycle, snowmobile, all terrain vehicles (ATVs), horse, or bicycle runs into an unseen wire or tree limb
- Strangulation
- Blows from fists or feet
- Excessive manipulation (eg, any force causing a realignment or repositioning of the spine including iatrogenic carotid or vertebral injury resulting from chiropractic treatment)







Well, this is interesting. I want to thank you for this great article. Thanks for sharing this :)
Trả lờiXóaback brace for men