Examination of the Oral Cavity
A thorough inspection of the oral cavity should be a part of any complete head and neck examination. Close visual inspection should be performed with adequate lighting, and each of the anatomic regions in the oral cavity should be palpated. Approximately 10% of patients who are examined have some abnormality of the oral mucosa. Some lesions can be diagnosed on the basis of the history and clinical findings alone. For other lesions, additional information may be required to properly guide any indicated therapy. Often, biopsy with ample tissue for microscopic analysis is the definitive procedure.
Management of Mucosal Abnormalities
The development of a reasonable differential diagnosis is of prime importance in determining if biopsy is indicated. Furthermore, the differential diagnosis aids the clinician in selecting the appropriate technique if biopsy is necessary.
A waiting period of 2 weeks often helps in forming the differential diagnosis because lesions that are related to infection, inflammation, or local trauma may resolve during this time. Biopsy is strongly recommended for the evaluation of most lesions that persist for 2 weeks or longer after the potential irritants are removed.
Conventional cytologic examination of the oral cavity is associated with an unacceptably high false-negative rate. However, for clinicians who are uncomfortable with intraoral surgery, brush biopsy with sampling of the full thickness of the mucosa may provide reliable information regarding the presence of cellular atypia. A positive result requires referral for scalpel biopsy.
Indications
Biopsy is indicated for the assessment of any unexplained oral mucosal abnormality that persists despite treatment or the removal of local irritants. Malignancy is suspected when persistent oral mucosal lesions are red or red and white or when they are ulcerated, indurated, or fixed to deeper tissues. Persistent lesions that bleed easily or grow rapidly should also alert the clinician to the possibility of malignancy. Unexplained pigmented oral lesions are of concern if they are new or changed. Biopsy is recommended unless the pigmented area has been present and unchanged for 5 years or longer.
Scalpel biopsy may be warranted even when the differential diagnosis includes only benign entities. Lesions that interfere with function and those that have an undesirable effect on esthetics should be excised.
Even experienced clinicians have difficulty in distinguishing truly innocuous oral mucosal changes and those that represent dysplasia or early invasive cancer. Therefore, the decision to forego biopsy in an apparently benign lesion should be made with great care and only when the patient understands the need for close follow-up and agrees to comply.
Also see the eMedicine article Cancers of the Oral Mucosa.
Contraindications
Oral mucosal biopsy has few contraindications. The standard biopsy techniques may require modification in some patients, including those with conditions that preclude the safe use of local anesthetic and those with severe bleeding diatheses or coagulopathies. Invasive procedures that may stimulate bone should be avoided when possible, or conducted with great caution in patients who have used or are currently using injectable bisphosphonates. Mucosal lesions in these individuals may be reflective of underlying osteochemonecrosis, a condition that may be exacerbated by any manipulation.
Technique Selection
A differential diagnosis is formed by reviewing the features of the history and physical findings in the context of the clinician's experiences and knowledge. The result should be a group of possible diagnoses, beginning with the most likely one. If the differential diagnosis includes malignancy, a tissue specimen must be obtained. Incisional biopsy is indicated in this situation so that definitive treatment of the potential malignancy is not compromised. If the differential diagnosis does not include malignancy, lesions of reasonable size in manageable locations can be completely excised at biopsy.
A variety of authors have proposed size limits for excisional biopsy. General dentists, dermatologists, oral and maxillofacial surgeons, otolaryngologists, and others undoubtedly have different comfort and skill levels; therefore, specific size guidelines for incisional biopsy versus excisional biopsy have little value. Similarly, clinicians who are uncomfortable with the regional anatomy should not perform excisional biopsy of lesions near significant anatomic structures. When excisional biopsy is being considered, the physician should also be aware that it may produce esthetic compromise as a result of scarring or residual deformity. The esthetic outcome is of particular concern when a lesion on the lip is near the vermilion border.
Numerous methods can be used to collect tissue samples from the oral mucosa for histopathologic examination. Performing biopsy with a scalpel is the standard and generally produces the most satisfactory specimen. Other techniques include the use of a needle, biopsy punch, biopsy forceps, laser, or electrocautery device. Needles may be appropriate in sampling cells from mass lesions, but they are of no benefit in the evaluation of surface lesions. Electrocautery produces thermal damage and artifact, which make evaluation of the specimen difficult; therefore, electrosurgery should be avoided during oral mucosal biopsy. Electrosurgery may be of benefit for wide local excisions of known intraoral malignancies after a scalpel is used to atraumatically obtain marginal specimens for frozen sections.
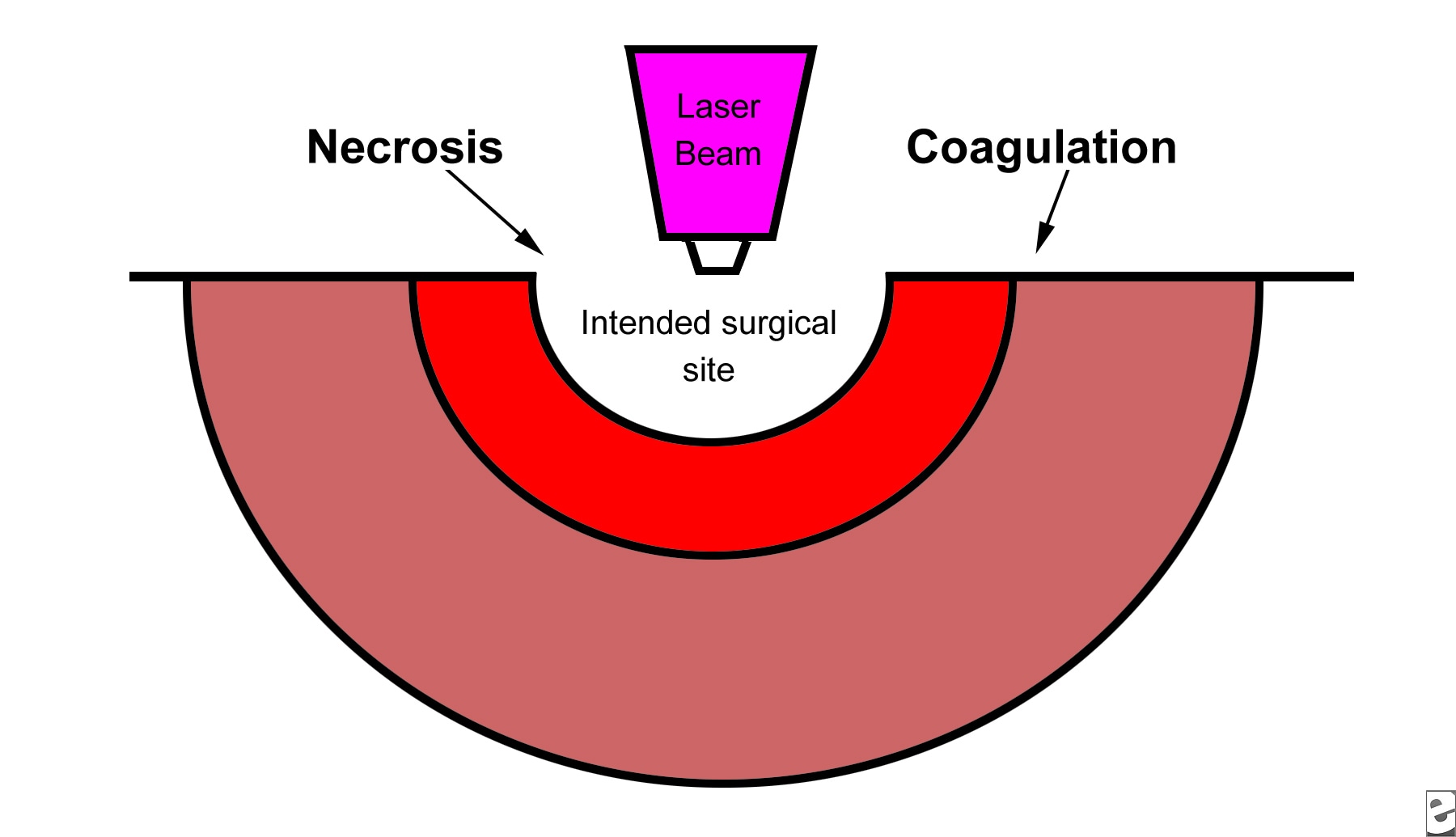
A carbon dioxide or Nd:YAG laser produces a zone of thermal coagulation smaller (approximately 500 µm) than that of electrocautery (see Media File 1).
If a laser is used for incisional or excisional biopsy, a 0.5-mm margin should be maintained between the cut and the representative area to be sampled. Although this technique may result in good local hemostasis and minimal postoperative discomfort, it is associated with potential shortcomings, including impingement on the specimen, particularly at the deep margin, and the generation of excessive heat with inadequate removal of the charred layer. The laser may be of great value in managing the wound left by scalpel biopsy in areas of the mouth where closure is difficult or inappropriate.
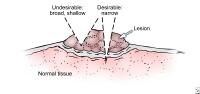
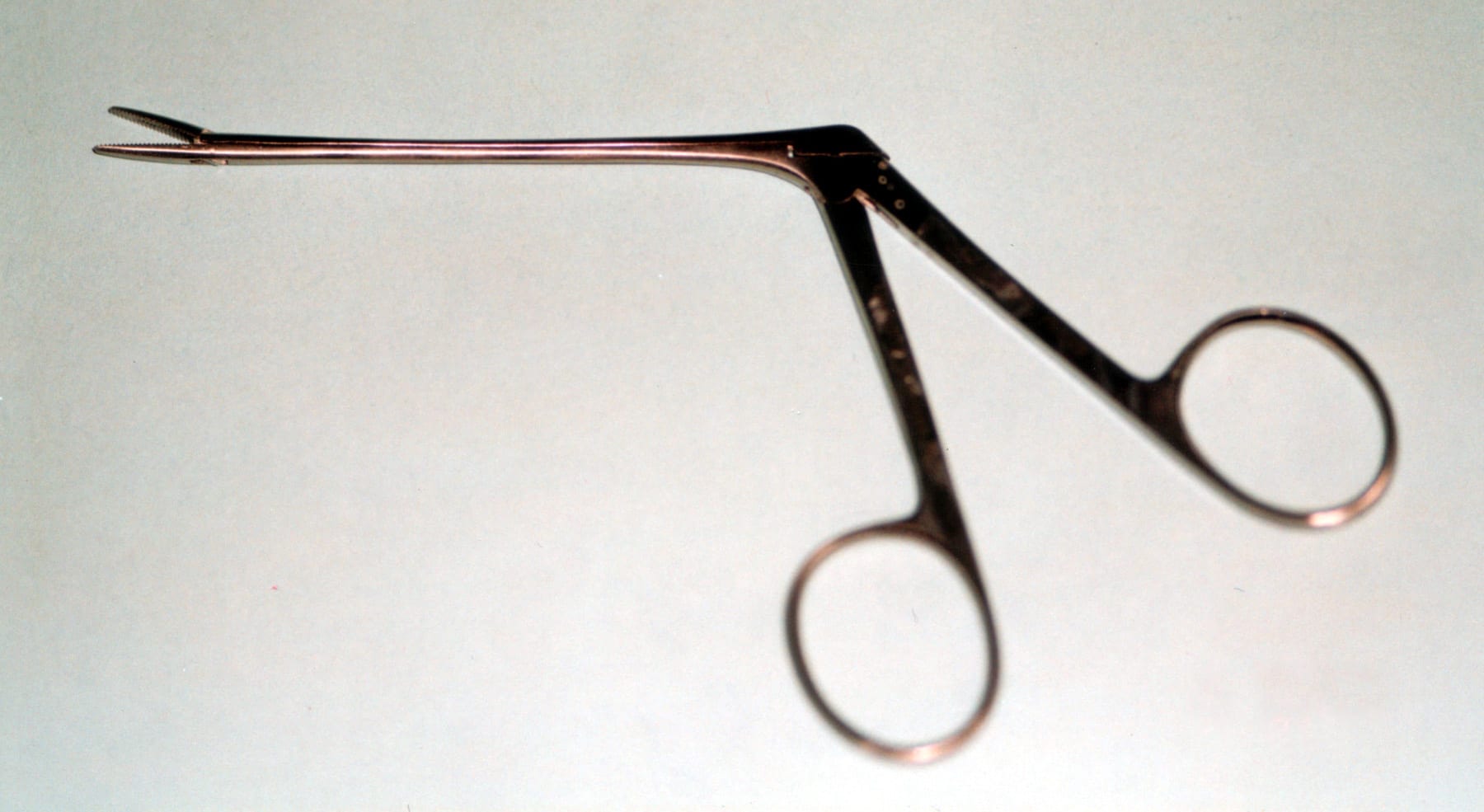
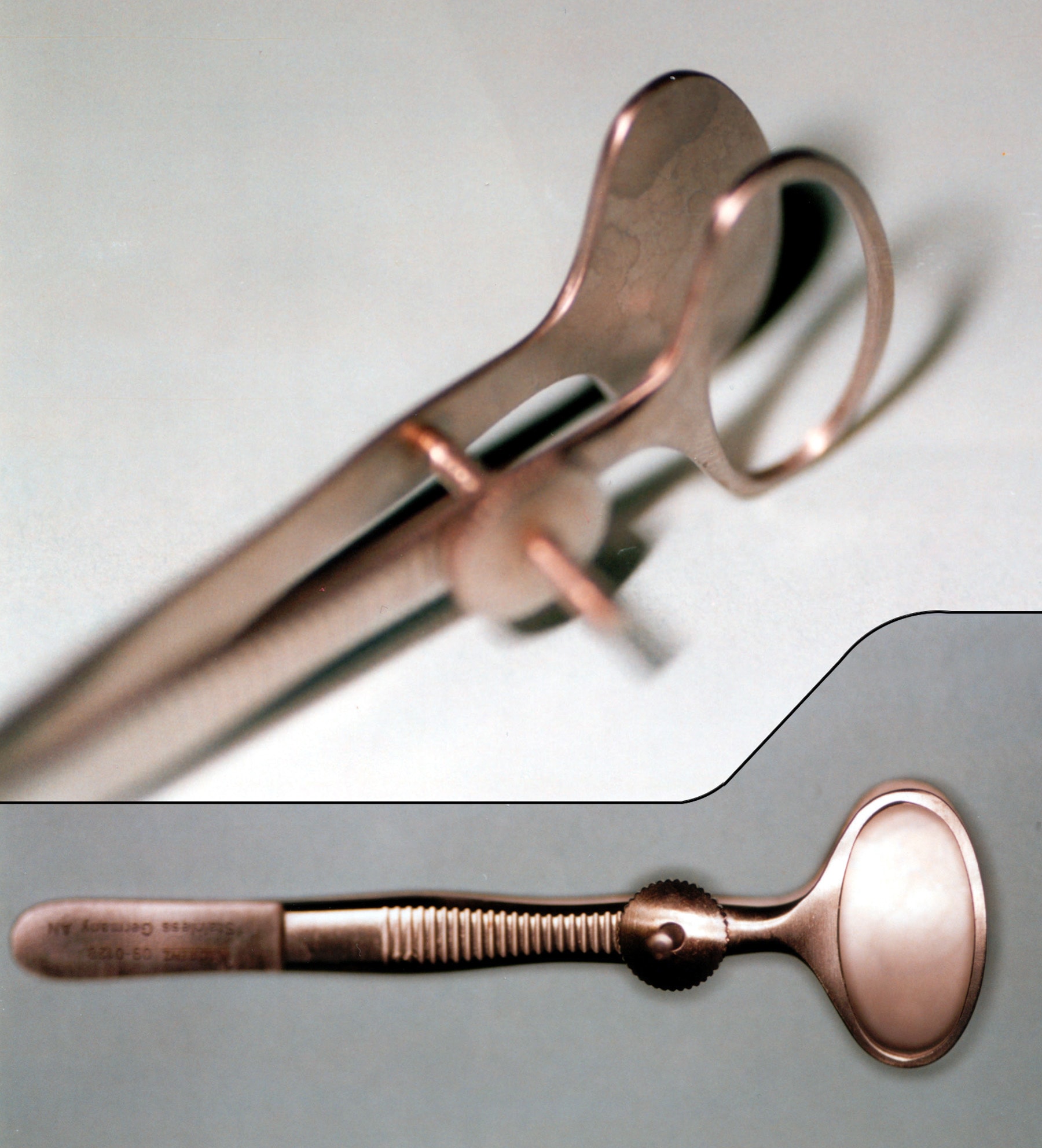
Biopsy forceps are long-handled instruments with biting ends that are cup shaped to harvest an adequate amount of mucosa. They are particularly useful in pharyngeal lesions for which the use of a scalpel is more challenging. The specimen is not crushed in the cup and should be eminently assessable by the pathologist (see Media File 2).
The use of a biopsy punch in oral mucosal lesions is described and may be of some value. Punch biopsy may be difficult on freely movable oral tissues and probably offers no advantage compared with scalpel biopsy (see Media File 3). The technique may be appropriate in the hard palate and other sites with better support and tissue that is bound down, and it is likely to produce a satisfactory specimen. The wound heals by secondary intention, and discomfort may persist longer than anticipated by the clinician and the patient.
Incisional biopsy
When incisional biopsy is contemplated, the biopsy site should be carefully considered. Much has been written about selecting a site at the periphery of a lesion to ensure the inclusion of healthy tissue. This site selection is certainly important in an ulcerated oral lesion. Selecting only the center of an ulcer results in an inadequate specimen devoid of mucosa. Some authors generalize this principle to nonulcerated lesions as well. Advocates of this approach might argue that the edge of many lesions is an area of activity and interest; however, the concept that the specimen must contain healthy tissue for pathologic diagnosis probably has little merit. The overriding principle that guides site selection for incisional biopsy should be the acquisition of the most representative sample of the suspected pathologic condition. An overzealous attempt to include the periphery of a lesion with clinically healthy tissue may inadvertently lead to a missed diagnosis or an underdiagnosis.
Persistent diffuse color and texture changes on oral mucosal surfaces may be the clinical expression of oral epithelial dysplasia. Specimens of similarly affected mucosa may yield adjacent zones of mild-to-severe dysplasia, carcinoma in situ, and microinvasive squamous cell carcinoma.1 This result raises the question of how a clinician knows whether incisional biopsy samples are sufficient for the most important histologic diagnosis of a diffuse area of mucosal change. Incisional biopsy can lead to a diagnosis of mild or moderate dysplasia despite the presence of invasive cancer within millimeters of the biopsy site. Therefore, a diagnostic adjunct may be used to guide the clinician to the biopsy site that is most likely to be associated with carcinoma in situ or invasive cancer.
One such adjunct is staining with toluidine blue (tolonium chloride), a dye that predictably stains affected mucosa and not unaffected areas. A significant body of evidence supports the effectiveness of this vital staining technique as a tool to enhance the diagnostic abilities of even experienced clinicians.2,3,4 A recommended protocol begins with careful assessment of the lesion in question on the first day. Potential irritants that may provoke an inflammatory response are removed for 2 weeks. Loose dentures, sharp spots on tooth cusps or dental prostheses, and parafunctional habits may all result in mucosal inflammation that can be clinically indistinguishable from an early oral cancer.
On the return visit in 14 days, the area is reevaluated. Persistent mucosal abnormalities, particularly those with red components, are stained by using an application technique. A few drops of toluidine blue are applied to the lesion and surrounding mucosa. Patients then rinse their mouths several times with water or a mild acetic acid solution. The dorsum of the tongue retains some stain because of its rough papillary contour.
On the remaining surfaces of the oral mucosa, any dark staining that persists and cannot be wiped off indicates the need for incisional biopsy. Biopsy should be focused on the area of greatest staining. Toluidine blue does not interfere with routine histopathologic examination nor does it hamper computer-assisted cytologic screenings of brush biopsy samples. Following this protocol, the sensitivity and specificity of toluidine blue staining are more than 90%. When properly applied, toluidine blue staining is a highly sensitive and specific test for carcinoma in situ and invasive oral cancer.
Chemiluminescent light based systems (ViziLite Plus, MicroLux DL, Orascoptic DK) use the application of a diffuse chemiluminescent light source to visualize abnormal oral mucosa not visible under normal incandescent light. After a 1% acetic acid oral rinse to remove surface debris and slightly desiccate the oral mucosa, cells with abnormal nuclear structure are purported to preferentially reflect the low-energy blue-white light emitted.10 Under illumination, normal epithelium absorbs the light, appearing light blue, while abnormal tissue reflects the light and appears white, with sharper, more distinct margins. Toluidine blue, discussed above, is used as a stain to aid in further lesion assessment (see Media File 12).
Tissue autofluorescence–based systems (VELscope) rely on the exposure of oral epithelium to specific wavelengths of light in order to produce an emission of energy in the form of fluorescence. The proposed mechanism of this fluorescence is related to reflective and absorptive patterns due to naturally occurring fluorophores in the oral mucosal tissue. This fluorescence is variable and it is affected by changes in tissue metabolism and structure. Further, the presence of hemoglobin, vessel dilation, and inflammation in the examined tissue can affect its appearance. Illuminating oral tissues with the VELscope device (see Media File 13) causes normal mucosa to emit a pale green light, whereas abnormal mucosa appears dark in presentation.
While these modalities may be useful adjuncts in the detection of oral lesions, the most definitive evaluation method for potentially malignant tissue is still a biopsy that provides the pathologist with an adequate sample of tissue in which the architecture has been preserved.11
Large diffuse zones of persistent mucosal change require multiple incisional biopsies. Close observation and/or repeat biopsy are indicated for areas diagnosed as mild or moderate dysplasia. Severe dysplasia, carcinoma in situ, and invasive cancers should be treated by using the principles of oncologic surgery.
The administration of local anesthetic for incisional biopsy is generally simple and straightforward. A small amount of local anesthetic infiltrated in an area peripheral to the lesion provides adequate anesthesia in nearly every situation. To avoid distorting the lesion, the anesthetic should not be injected directly into it. Theoretically, direct injection can also result in an inadvertent seeding of cells deeper into the tissues. The judicious use of a vasoconstrictive agent in the anesthetic solution improves local hemostasis and can be helpful when indicated.
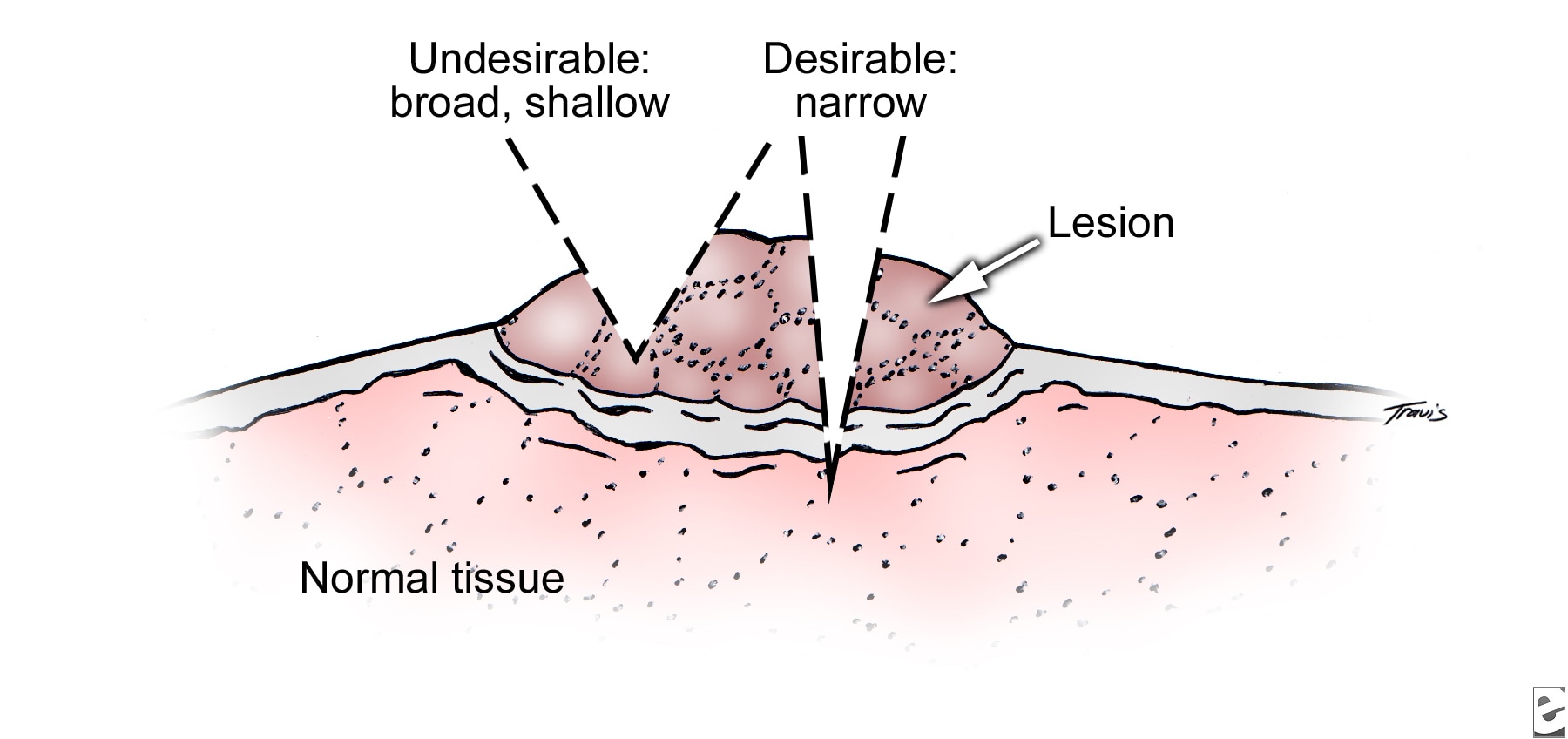
The minimal requirements for an adequate specimen vary somewhat with the nature of the pathologic entity. As a general principle, including tissue subjacent to the epithelium and removing a wedge of manageable size is desirable. Therefore, a minimal depth of 3 mm, minimal length of 3-6 mm, and minimal width of 1-2 mm are advised (see Media File 4).
As with excisional biopsy (discussed below), suction devices should be used with caution or completely avoided to prevent inadvertent loss of the specimen. If necessary, a suction tip covered with gauze safely keeps the field clear.
The physician's armamentarium for biopsy includes the following:
- Blade handle with a No. 15 blade
- Fine tissue forceps with teeth
- Local anesthetic solution and syringe
- Retractor appropriate for the site
- Suture for traction, if needed
- Needle holder
- Suture for closure, if indicated
- Fine-tipped scissors
- Laser or electrocautery device for fulguration, if indicated
- Specimen bottle containing formalin and biopsy data sheet
- Gauze sponges
Small wedge-shaped incisional biopsy sites can usually be closed with a single suture. Small wounds in the floor of the mouth or on the tonsillar pillars heal well without primary closure. Hemostasis may be achieved by using a laser or electrocautery unit if necessary.
Excisional biopsy
Given a differential diagnosis that includes only benign entities, the clinician may elect to remove a lesion in its entirety. As indicated previously, the size of the lesion is only one of several factors that may affect the decision to perform excisional biopsy. The location of the lesion, the nature of its attachment to the underlying tissue, the accessibility of the lesion, and the regional anatomy all contribute to the decision. Small, pedunculated, exophytic masses in accessible areas are excellent candidates for excisional biopsy.
The preferred methods for the administration of local anesthetic are regional blocks or field blocks, which are accomplished by means of infiltration peripheral to the lesion. Much of the oral mucosa is easily movable, and an assistant may need to stabilize the area by using an instrument or his or her fingers. Stabilization and traction techniques specific to the various anatomic area within the oral cavity are discussed in Special Considerations below.
As with incisional biopsy, suction devices should be used with caution or completely avoided during excisional biopsy to prevent inadvertent loss of the specimen. If necessary, a suction tip covered with gauze safely keeps the field clear. When excisional biopsy is planned, the lines of excision should ensure that the entire lesion is removed.
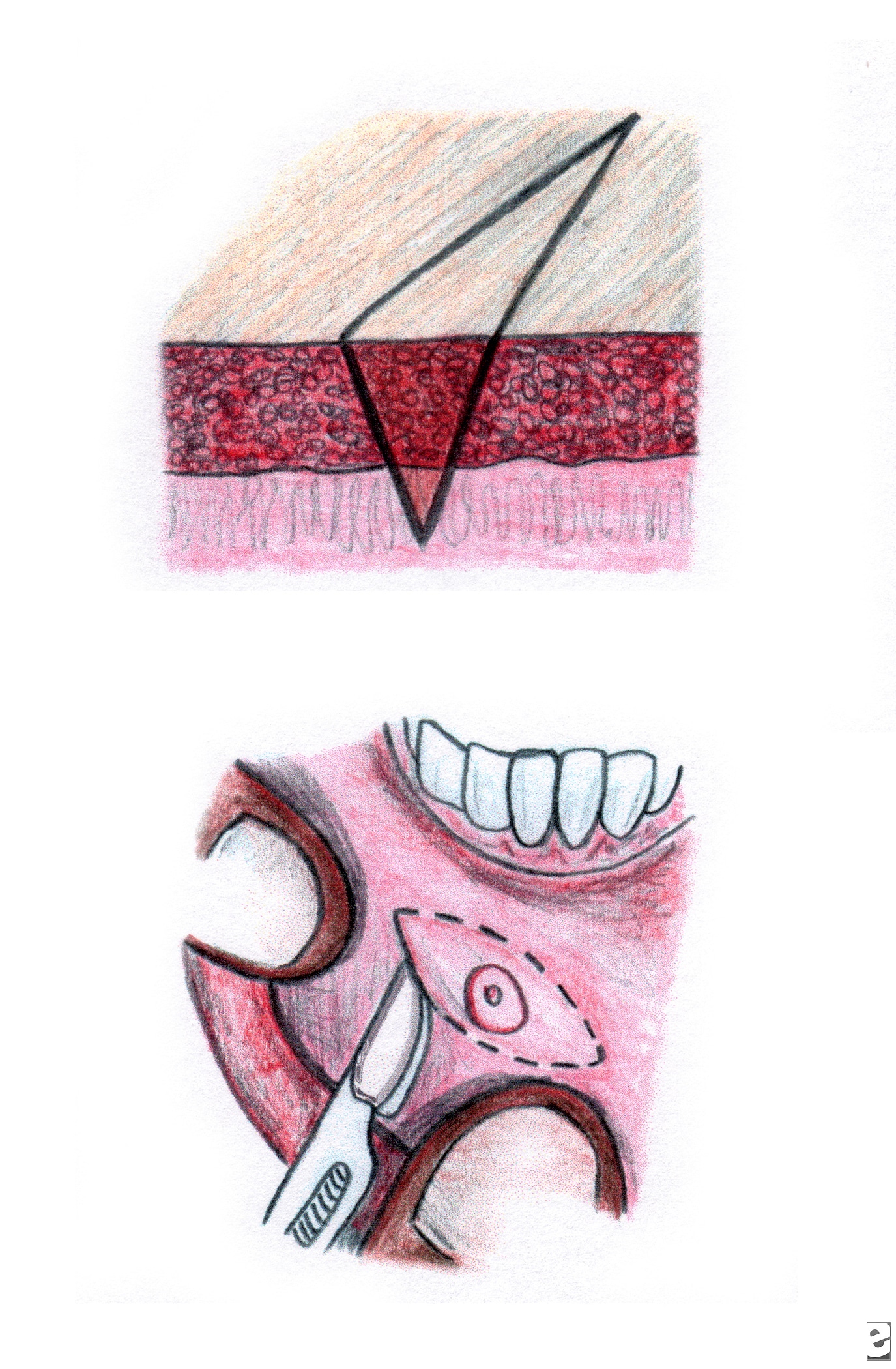
Two incisions forming an ellipse are made around the lesion with the blade angled toward the lesion. These incisions produce a wedge-shaped specimen that is deepest under the center of the lesion and leaves a wound that is simple to close Closure is facilitated by developing an ellipse that is 3 times longer than it is wide (see Media File 5). In general, properly designed elliptical wounds can be closed easily; however, depending on the location of the biopsy site and the size of the wound, mucosal undermining may help in producing a tension-free closure.
View from above (top) and in cross section (bottom) shows the wedge-shaped specimen with a length-to-width ratio of 3:1.
The physician's armamentarium for biopsy includes the following:
- Blade handle with a No. 15 blade
- Fine tissue forceps with teeth
- Local anesthetic solution and syringe
- Retractor appropriate for the site
- Suture for traction, if needed
- Allis forceps
- Needle holder
- Suture for closure, if indicated
- Fine-tipped scissors
- Laser or electrocautery device for fulguration, if indicated
- Specimen bottle containing formalin and biopsy data sheet
- Gauze sponges
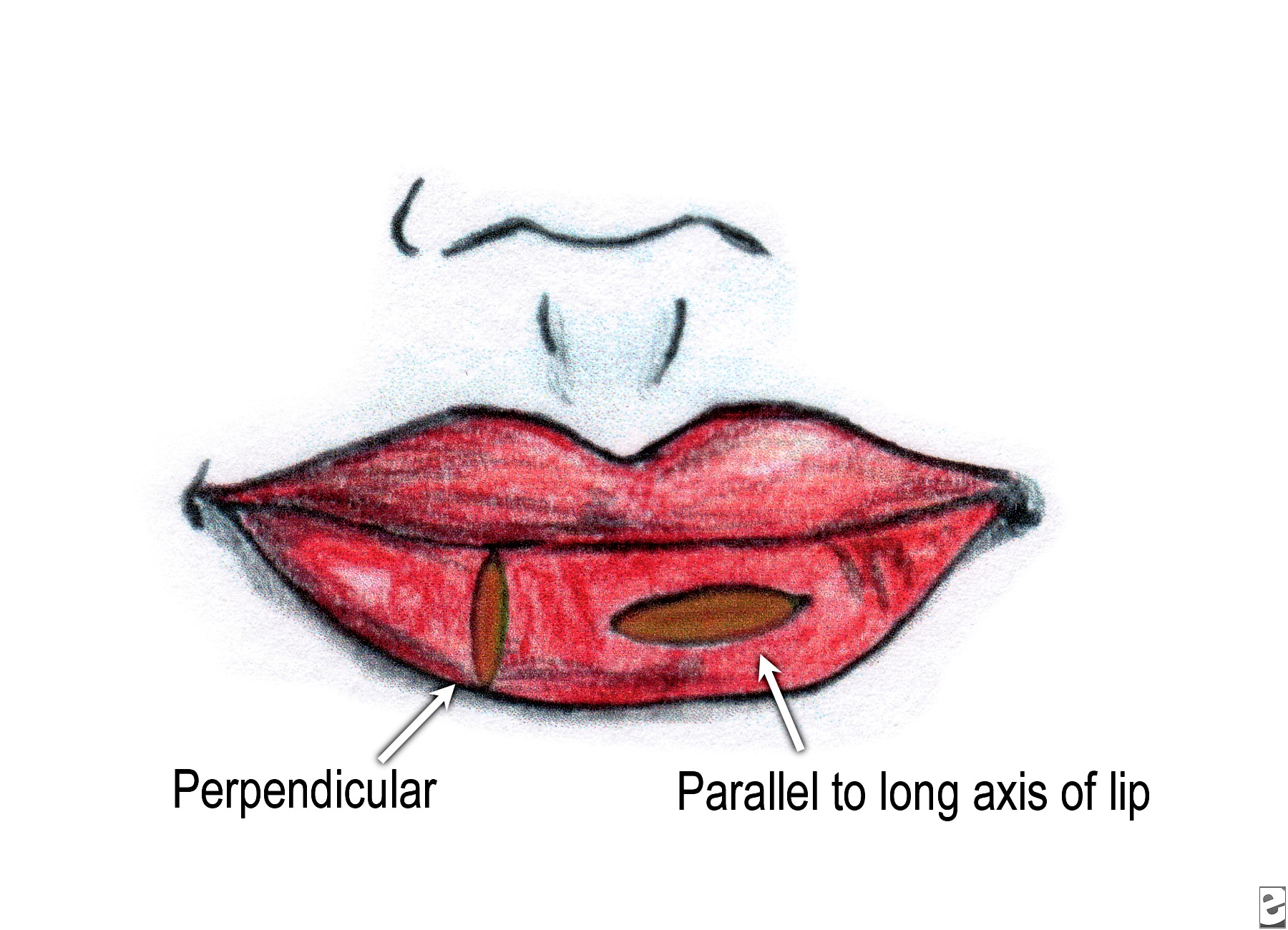
Special Considerations
The excision of lip lesions requires planning and tissue stabilization. In general, excision lines should be parallel to the nerves and vessels; however, a substantial excision from the lip parallel to its long axis may result in a decrease of visible vermilion after healing. The white roll of the lip may be pulled in because of the loss of tissue and contracture during healing. Although this excision is unlikely to produce a major deformity, the esthetics may be compromised. Excisions made perpendicular to the long axis of the lip are far less likely to produce this type of distortion; however, with the 3:1 rule (ie, the specimen should be 3 times longer that it is wide), the excision of a lesion near the vermilion border requires the clinician to cross onto the skin to produce a wound that can be closed properly. This incision may result in a scar that is more visible and more troublesome to the patient than one confined to only the labial mucosa (see Media File 6).
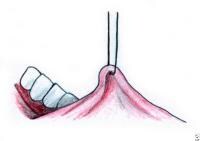
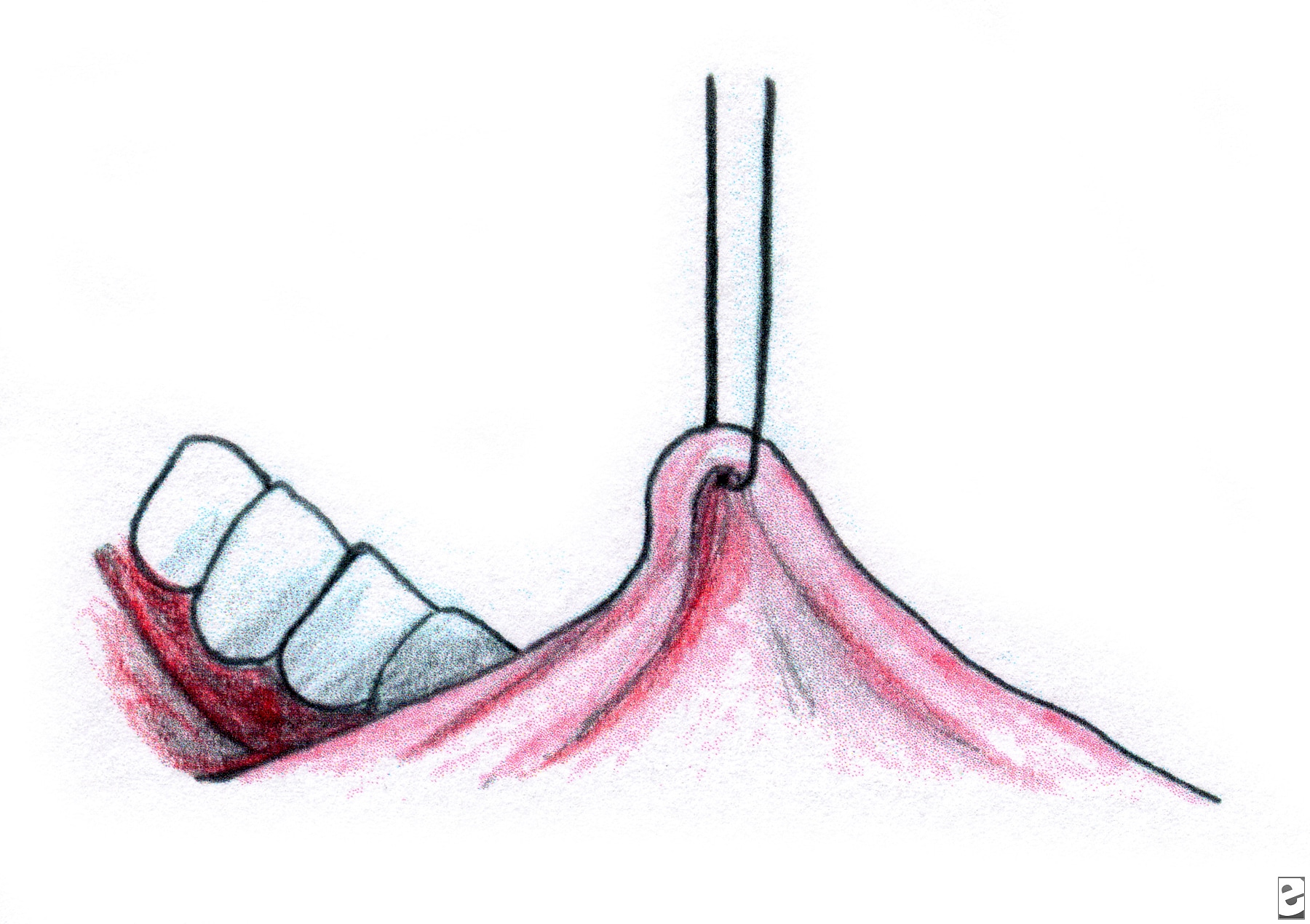
Excisional biopsy of the lip may be difficult to perform without assistance. Bleeding can obscure the field, and the mobility of the labial tissues further complicates what should be a simple procedure. Local hemostasis and tissue stabilization are managed better if the clinician and an assistant each firmly grip the lip by placing their thumb and index finger on either side of the lesion (see Media File 7). This clamping occludes the labial artery and its local branches and immobilizes and tenses the tissue. Another approach is to use a chalazion clamp, which reduces bleeding, tenses and stabilizes the tissue, and provides the operator with a convenient handle so that control can be maintained throughout the procedure. After the specimen is removed from the field, the chalazion (see Media File 8) is loosened slowly and carefully, and any bleeding sites are addressed before the wound is closed.
Tongue lesions present similar difficulties. An assistant can stabilize the tongue by wrapping the tip in a gauze sponge and grasping it firmly. Alternatively, heavy sutures or towel clamps can be used to control the tongue after appropriate local anesthesia is achieved (see Media File 9). When tongue wounds are closed, deep sutures should be placed when indicated, and mucosal sutures should be placed fairly close to each other. Inadequately closed wounds on this movable and highly vascularized organ tend to re-open, with resultant oozing and/or delayed healing.
A different set of issues arises when excision is planned for a lesion that appears to emanate from the keratinized attached gingiva. A periodontist or oral and maxillofacial surgeon should evaluate and manage these lesions. A number of pathologic entities that appear to arise from the gingiva are actually derived from the periodontal ligament. Recurrence is more likely in these lesions if their true origin is not addressed. In addition, even the appropriate excisions of small amounts of attached gingiva may result in significant periodontal defects.
Lesions on the hard palate and remote from teeth may be safely excised as long as attention is paid to the underlying vascular anatomy. Because keratinized oral tissues are tightly bound to the skeleton, denuded bone may remain after this type of excisional biopsy is performed. Inform the patient that denuded bone in the oral cavity can cause discomfort for several weeks. Even if bone is not exposed, resultant wounds that involve the attached gingiva and palate are generally not closed primarily.
Specimen Handling
Surgical specimens obtained with any of the biopsy techniques discussed above should be handled appropriately. During the biopsy procedure, the lesion is grasped with an Allis forceps or secured with a traction suture (see Media Files 10-11). The use of any instrument that crushes the specimen makes the pathologist's work more difficult, if not impossible. The specimen should be removed from the field and placed into a solution of 10% formalin. The volume of formalin should be at least 20 times the volume of the specimen.
Special tests may require that a second specimen be submitted in a different solution. For example, in the diagnosis of lesions possibly related to an autoimmune process, immunofluorescent studies may be of value, in addition to standard hematoxylin and eosin staining. Specimens for direct immunofluorescence testing must be submitted in Michel solution.
Communication and Summary
Communication
Thorough documentation is essential, and the patient's record should include a description of the lesion and its location, as well as a diagram to illustrate the chart entry. Any lesion that is being followed up should be photographed. Data gathering may involve radiography, vital staining, and other modalities, the result of which should be appropriately documented. Any information that may assist the pathologist in making a diagnosis should be included on the biopsy report. The surgeon should be encouraged to review the histopathology slides, particularly when malignancy is diagnosed or when the microscopic and clinical assessments differ.
Summary
The indications and techniques for oral mucosal biopsy are similar to those for biopsy of the skin. However, significant differences exist, and some site-specific recommendations are reviewed here. The most important principle is to never ignore a persistent oral mucosal abnormality.
For excellent patient education resources, visit eMedicine's Cancer and Tumors Center. Also, see eMedicine's patient education article Cancer of the Mouth and Throat.
Multimedia
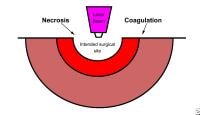 | Media file 1: Diagram illustrates thermal damage zones caused by carbon dioxide laser. |
 | Media file 2: Biopsy forceps. |
 | Media file 3: Biopsy punch. |
 | Media file 4: Acquisition of a sample at incisional biopsy. |
 | Media file 5: View from above (top) and in cross section (bottom) shows the wedge-shaped specimen with a length-to-width ratio of 3:1. |
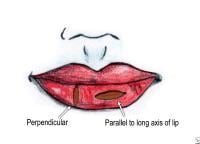 | Media file 6: Diagram shows the elliptical excisions parallel and perpendicular to the long axis of the lip. |
 | Media file 7: The lip is being held by a clinician and an assistant. |
 | Media file 8: Chalazion clamp. |
 | Media file 9: The tongue is being stabilized for biopsy. |
 | Media file 10: Traction suture. |
 | Media file 11: Allis forceps. |
 | Media file 12: ViziLite kit. |
 | Media file 13: VELscope machine. |
Keywords
oral punch biopsy, oral scalpel biopsy, oral biopsy, incisional biopsy, excisional biopsy, biopsy punch, biopsy forceps, management of mucosal lesions, indications for biopsy of oral lesions, mucosal abnormalities, examination of the oral cavity
The authors and editors of eMedicine gratefully acknowledge the contributions of previous author, Antonio Locantore, DDS, and previous Chief Editor, William D. James, MD, to the development and writing of this article.
More on Oral Punch Biopsy and Scalpel Biopsy |
| References |







Hi Very Nice Blog I Have Read Your Post It Is Very Informative And Useful Thanks For Posting And Sharing With Us And Your Writting Style Is Very Nice
Trả lờiXóamaxillofacial instrument
Hi Very Nice Blog I Have Read Your Post It Is Very Informative And Useful Thanks For Posting And Sharing With Us And Your Writting Style Is Very Nice
Trả lờiXóamaxillofacial instrument
I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóaHOW DR IMOLOA HERBAL MEDICINE HELPED ME GET RID OF MY 3 YEARS HERPES SIMPLEX VIRUS. Hello everyone my name is DONALD am from the united states i have been suffering from (HERPES) disease since 2016 and had constant pain, especially in my knees. During the first year,I had faith in God that i would be healed someday.This disease started circulate all over my body and i have been taking treatment from my doctor, few weeks ago i came on search on the internet if i could get any information concerning the prevention of this disease, on my search i saw a testimony of someone who has been healed from (Hepatitis B and Cancer) by this Man Dr Imoloa and she also gave the email address of this man and advise we should contact him for any sickness that he would be of help, so i wrote to Dr imoloa telling him about my (HERPES Virus) he told me not to worry that i was going to be cured!! hmm i never believed it,, well after all the procedures and remedy given to me by this man few weeks later i started experiencing changes all over me as the Doctor assured me that i have been cured,after some time i went to my doctor to confirmed if i have been finally healed behold it was TRUE, So friends my advise is, if you have such sickness or any other at all like, FEVER, DIARRHOEA, LUPUS, DRY COUGH, MOUTH ULCER, MOUTH CANCER, SKIN CANCER, PANCREATIC CANCER, PENILE CANCER, JOINT PAIN, BONE CANCER, PRAKISON'S DISEASE, FATIGUE, MUSCLE ACHES, ANAL CANCER, ARTHRITIS, BREAST CANCER, BONE CANCER, hepatitis A,B,C,CANCER,HPV,HIV/AIDS,DIABETES 1 AND 2,SMALL PENIS PROBLEM ,HIGH BLOOD PRESSURE SYPHILIS, WEAK ERECTION,BREAST ENLARGEMENT AND many more ....... you can email him on drimolaherbalmademedicine@gmail.com) or whatsapp him on +2347081986098. Sir, i am indeed grateful for the help i will forever be grateful for the good work.
Trả lờiXóa