Introduction
Trauma is the leading cause of death in children. Pediatric trauma patients admitted to the hospital have a 5% incidence of facial fractures. Pediatric trauma patients differ from their adult counterparts. Patterns of injury, treatment algorithms, and potential consequences of facial trauma and its treatment are affected by the physiology of facial growth and development.
For excellent patient education resources, visit eMedicine's Breaks, Fractures, and Dislocations Center and Teeth and Mouth Center. Also, see eMedicine's patient education articles Facial Fracture and Broken or Knocked-out Teeth.
History of the Procedure
Kaban's 1993 review of the history of treatment of pediatric facial fractures during the period from 1943-1993 highlights several changes.1 Although seat belts were not in use during the early part of this era, overall traffic speed and frequency of car travel were much lower than today. Today, with advances in critical care and trauma medicine, more children survive high-impact accidents. Previously, many children died of associated injuries. Medical management of these patients also improved with the increase in development and availability of antibiotic medications. Surgical management of facial fractures improved and continues to improve with advances in rigid fixation, including the relatively recent advent of resorbable plating systems.
Frequency
The incidence of facial fractures is lower in the pediatric population than in the adult population.2 Reported incidence of facial fractures in the pediatric age group approximates 5% of all facial fractures. In Rowe's 1968 series of 1500 facial fractures, less than 1% of fractures occurred in children younger than 5 years.3 Incidence in children aged 6-11 years was 4%. These numbers are consistent with McCoy's 1966 series of 1500 facial fractures, in which 6% of patients were aged 14 years or younger.4 Facial fractures in the pediatric patient are more difficult to diagnose than in the adult patient. Physical examination findings are less accurate, and these patients are less able to communicate their symptoms. In addition, fractures heal quickly; therefore, a significant portion of these fractures may escape diagnosis, particularly if the fractures are nondisplaced. The 2 studies were completed before the widespread use of CT scanning.
Although in Posnick's 1993 series of 137 patients the group most frequently involved was aged 6-12 years, most studies show a general trend toward an increased fracture rate with increasing age.5 Fractures in children younger than 1 year are rare, and the fracture rate among the youngest group remains low. About 10% of fractures in children occur in those younger than 4 years. A male predominance has been documented in patients with nasal or blowout fractures, but an equal incidence between the sexes seems to exist in patients with mandibular fractures. Males are overrepresented when the etiology is interpersonal violence or most sporting activities. The sex bias diminishes with the increase of motor vehicle collisions as an etiology. The decreased incidence and unique pattern of facial fractures in children are affected by the protected environment and developing facial anatomy of the child.
Etiology
Children younger than 5 years are usually supervised continuously. While developing new skills and exploring, falls occur frequently but are from a low height and do not generate much force. After age 5 years, children become more independent; they leave close supervision and begin to engage in sports and recreational activities such as riding bicycles, playing ball games, and climbing playground equipment.6 The teenage years involve further risk-taking and a dramatic increase in interpersonal violence.
In most recent studies, the leading etiologic factor of facial fractures is motor vehicle collisions. The etiology appears to vary by age. The most common factor in patients younger than 3 years is falls. In those aged 3-5 years, traffic accidents barely exceed falls. By adolescence, recreational activities and interpersonal violence are second to motor vehicle collisions. (Pedestrians struck by vehicles are usually included in the motor vehicle collision group.) In Kaban's 1993 series, motor vehicle collisions were the most frequent cause in children younger than 7 years, but falls were the most common cause in children of all ages.1
Although not a commonly reported cause, caregivers should be aware of child abuse as a potential cause of any pediatric injury. In McCoy's 1966 series of 86 pediatric patients with facial fractures, 12% were attributed to battering.4
Continued efforts at improving motor vehicle safety, including relatively new seat belt and car seat regulations, and traffic safety awareness for pedestrians, drivers, and cyclists should help prevent these injuries. In addition, schools should emphasize bicycle safety and routine use of protective equipment for sporting activities. Societal changes to decrease violent behaviors are crucial in preventing trauma in teenagers.
Pathophysiology
Knowledge of facial growth and development is important in understanding patterns of pediatric facial trauma and the rationale behind its treatment. Changes in facial shape and the development of the sinuses and dentition play crucial roles in the fracture pattern observed in the pediatric patient.
The human head doubles in size from infancy to age 5 years, reaching 80% of adult size by that time. The shape and projection of the face change dramatically during the first years of life. At birth, the face-to-cranium ratio is 1:8. This increases to 1:4 at 5 years and reaches the adult ratio of 1:2.5 during adolescence. The cranium increases 4 times, and the face increases 12 times from birth to adulthood.
The facial skeleton grows by a combination of displacement and remodeling. Displacement is the movement of bone in relation to the rest of the facial skeleton. Remodeling involves change in the shape of an individual bone by deposition at one side and resorption at another. Anatomic growth centers are well described; however, soft tissue covering and muscular pull also appear to be important influences in facial growth.
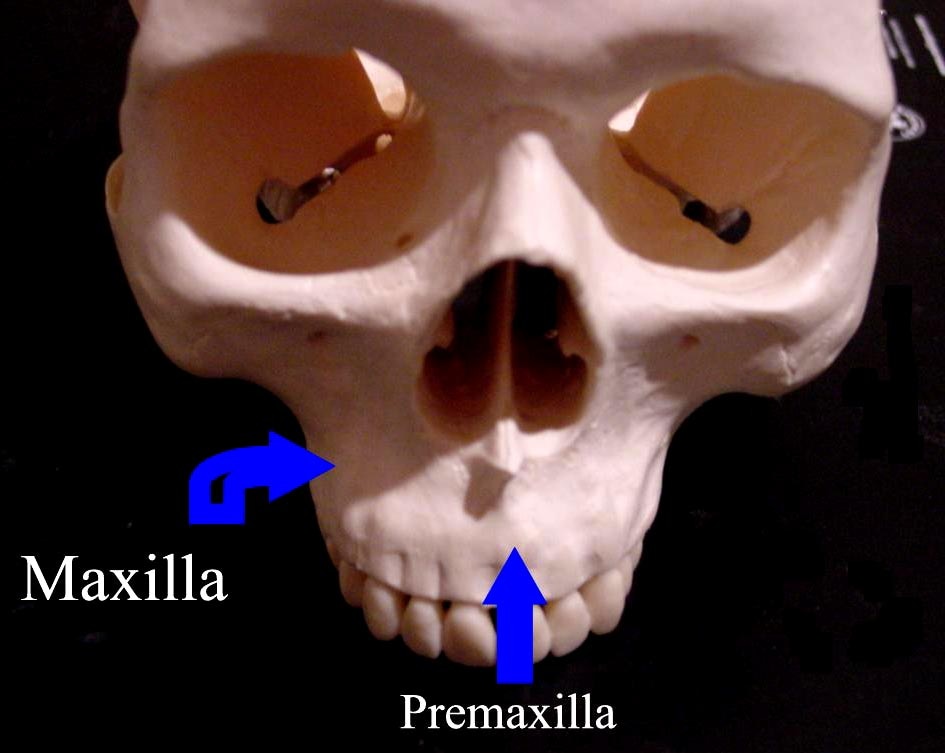
Growth of the nasomaxillary complex relates to growth of the cranial base. The face grows downward and outward by complex remodeling. The nasal septum is considered a coordinating center of midface growth. Studies in nonhuman primates have demonstrated midface hypoplasia after surgical resection of the septum. Most of midface growth occurs in the lower part of the midface. The lower maxilla grows in a vertical direction. The nasal cavity widens to mid orbit, and the floor of the cavity descends as the permanent dentition erupts.
The mandible in an infant is small and retruded. As it grows, it widens and lengthens the lower face. The condylar growth centers orchestrate mandibular development. Each growth center consists of a fibrous cap with an inner chondrogenic layer, a layer of cartilage, and a layer of ossifying cartilage. The infant mandible grows anteriorly and laterally, thus enlarging the lower face. Addition of bone at the condyle and posterior ramus and bony resorption anteriorly contributes to the forward projection. This process continues after most of the facial skeletal growth is complete; therefore, damage to the condyle has the potential to cause growth disturbances, but the continued growth may also confer a unique healing ability.
Sinus development begins with the maxillary sinus, which is first visible at age 5 months. The sinus enlarges over the first 5 years of life and descends below the floor of the nose with the eruption of permanent dentition at age 12 years. The maxillary sinus is developed fully at age 16 years. The ethmoid sinuses are first visible at age 1 year. The frontal sinus appears at age 6 years and reaches adult size by late puberty. Development of the sinuses directs the force of impact and may exert a cushioning effect.
The development of dentition also plays a crucial role in the treatment of pediatric facial fractures. Deciduous dentition erupts during the first 2 years of life. In children aged 6-12 years, these teeth are gradually replaced by permanent dentition. (This is the period of mixed dentition.) The presence of unerupted teeth confers some protection; however, when fractures do occur, they tend to run along tooth crypts. The status of dentition also affects the treatment of fractures. The youngest patients are edentulous. Deciduous teeth may be loose, and the shape of these teeth is not conducive to circumdental wiring.
In addition to the changing facial projections and growth of underlying sinuses and teeth, the structure of the bone is different in pediatric patients. Pediatric facial skeleton has more cartilage (cartilaginous growth centers) and a higher proportion of cancellous to cortical bone. The medullocortical junction is indistinct, causing an irregular fracture pattern. Bone in the young child is less mineralized and, therefore, more elastic. The overlying soft tissue also is relatively thick. All of these factors increase the incidence of greenstick fractures. The high rate of bone metabolism causes fractures to heal rapidly. Where appropriate, perform early intervention. Active and growing bone may also have the potential for remodeling.
With facial development, different anatomic areas become more vulnerable to injury. The infant's mandible and midface are relatively retruded and so are protected, whereas the frontal area is prominent and prone to injury. In adults and older children, the zygomaticomaxillary complex (ZMC), nasal, and Le Fort fractures become more common.
Presentation
Although facial injuries may be the most obvious, triaging patients who have these injuries as trauma patients is important to avoid missing more threatening injuries.
The airway remains the first priority in treatment of the trauma patient. Modest mucosal edema causes substantially more difficulty in the smaller airway of a child. Carefully suction blood and debris from the oropharynx. Fractures of the anterior mandible may cause the tongue to displace posteriorly. Obstruction caused by the retruded tongue can be managed with positioning or a traction suture; however, take care to ensure appropriate protection of possible cervical spine injuries. Orotracheal intubation may be necessary and is preferred over an emergent surgical airway.
Control of hemorrhage is the next priority. The face and scalp are quite vascular, and blood loss is proportionally greater in a child. Direct pressure on the site of bleeding usually controls bleeding. Expedient closure of scalp lacerations also is helpful.
The secondary examination is more difficult in a child. The patient is fearful after the accident and apprehensive of the hospital environment. Children frequently anticipate additional pain and are less able to articulate concerns. Older children may report abnormalities of occlusion and visual symptoms. A thorough examination begins with inspection of the face. Swelling, ecchymosis, and asymmetry are clues of underlying fractures.
Next, palpation of the face is performed in an orderly fashion, beginning over the cranial vault and then proceeding to the forehead, orbital rims, zygomatic arch, maxillary alveolus, and mandible. Asymmetry, irregularity, step-offs, crepitation, and tenderness may indicate a fracture. Palpation in the external auditory canal may reveal a condylar fracture. Bimanual palpation of the mandible may reveal step-offs and instability. Numbness in the infraorbital, supraorbital, and mental distributions may indicate transection or stretch of a nerve from a nearby bony injury.
Perform careful inspection of the nasal cavity to exclude a septal hematoma, which if found, should be drained promptly. Otoscopy may reveal a hemotympanum, indicative of a temporal bone or basilar skull fracture. Blood in the external auditory canal may be evidence of a condylar fracture. A condylar fracture with impaction through the glenoid fossa may result in an external auditory canal laceration. Inspection of the mouth for missing teeth, intraoral lacerations, and ecchymosis also is necessary. Ophthalmologic examination should include observation of pupillary reflexes, examination of gross visual acuity, testing for diplopia (when possible), and assessment of extraocular muscle movements. Formal ophthalmologic consultation is indicated for fractures involving any of the orbital structures and is crucial for preoperative documentation.
Associated injuries
Children with facial fractures have a high incidence of coexistent injuries. Injuries other than facial wounds occur in 55-60% of these children. In McCoy's 1966 series, 40% of facial fractures were associated with skull fractures.4 Two of the 86 patients had vertebral injuries. One third of children with facial fractures have injuries to other organ systems. Head injuries are most common, followed by extremity injuries. Interestingly, the rate of associated cervical spine injuries appears to be much lower than the 10-15% commonly reported from adult series. A positive association exists between the complexity of the facial fracture and the likelihood of an associated injury. Fractures of relatively protected and resilient bones generally are due to high impact; therefore, suspect concomitant injuries. Fifty-five percent of patients with orbital fractures have associated injuries (mostly neurocranial), but a third of these patients also have an orthopedic injury.
Indications
If fractures are displaced and a stable reduction cannot be achieved, perform a surgical reduction with rigid fixation (see Surgical therapy).
Relevant Anatomy
Distribution of fractures
The mandible and nasal bones are the 2 most frequent sites of fracture. Nasal fractures are typically managed in an outpatient setting and are excluded from many series. In Posnick's 1993 series, the most common type of fracture was mandibular, at 34%; followed by orbital, at 23%; and dentoalveolar, at 14%.5 Midface fractures were less common, at 7%. Approximately 90% of midface fractures and zygoma fractures occurred in children older than 6 years. In a 1968 report, Rowe found that only 10% of pediatric fractures involved the midface, and he found these fractures to be very uncommon in those younger than 8 years.3 Similarly, Dufresne reported mandible fractures to account for 32%, orbital fractures for 23%, and Le Fort fractures for 2.7% of pediatric fractures.7 Kaban's 1993 series (which included nasal fractures) demonstrated fracture distribution as 45% nasal, 32% mandibular, and 20% ZMC and orbit.1
Contraindications
See Surgical therapy.

very useful post...thanks for sharing.
Trả lờiXóahttp://dentallecnotes.blogspot.com/2011/07/note-on-use-of-resorbable-plates-and.html
I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóa