Introduction
Definitions
A skin flap consists of skin and subcutaneous tissue that survives based on its own blood supply. Skin flaps are classified by the source and pattern of that blood supply.1 The most basic of skin flaps are based on the nonspecific or "random" blood supply of the subdermal plexus. For more information, see Flaps, Classification.
Indications
Use a skin flap for wound coverage when inadequate vascularity of the wound bed prevents skin graft survival. Use skin flaps for functional and cosmetic requirements for wound coverage on the face, particularly around the eyes, nose, and mouth. Skin flaps are indicated when specialized tissue is needed to cover gliding tendons, for bulk tissue to fill contour defects, and for specialized sensory function.
History
The earliest flaps were random flaps, such as the random pedicled flap (from the upper arm to the nose) described by Tagliacozzi in the 1500s. Other important contributors to the history of skin flaps include von Graefe in 1818, Mutter in 1843, Dieffenbach in 1845, and Gersuny in 1887. Gilles and Fillatov described the tubed pedicle flap in the early 1900s. These flaps were limited by their length-to-width ratios of 5:1 for the face ranging to 1:1 for the lower extremity. As described by Blair in 1921, only by delaying a flap could a surgeon exceed that length-to-width ratio.2
Manchot defined the vascular patterns of skin circulation in 1889,3 and Davis demonstrated axial and pedicle flaps in 1919. In 1965, Bakamjian described the deltopectoral flap and reintroduced arterial flaps based on the initial efforts of Esser.4 In 1970, Milton demonstrated that flap survival was based not on the length-to-width ratio but rather on the blood supply that was incorporated into the flap.5 In 1973, Daniel defined the source of the blood supply as either the musculocutaneous or direct cutaneous vessels.
With increased understanding of the blood supply to flaps, the delay technique was used less commonly.6 Many new flaps were described, including muscle flaps and fasciocutaneous flaps. Some flaps previously described as random flaps, such as Indian forehead flap described in the 1440s for nasal reconstruction and Gilles's abdominal tube pedicle flap, were found to be based on known direct cutaneous vessels (ie, supratrochlear artery for the forehead flap, superficial epigastric artery for the abdominal flap). With the introduction of the operating microscope, flaps were no longer restricted by location and could be transferred to any part of the body using microvascular techniques (see Flaps, Free Tissue Transfer).2
Method of Flap Movement
Skin flaps can be moved to a local or distant site.
Local flaps
Use local flaps for defects that are adjacent to the donor site. The types of local flaps are based on the predominant type of movement.2
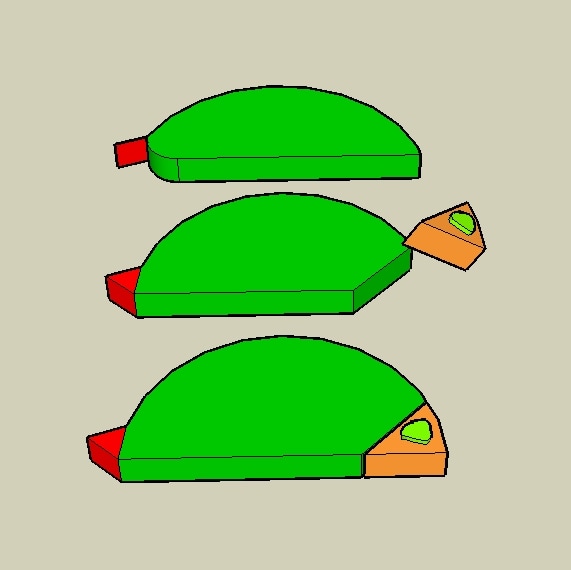
An advancement flap, shown below, moves directly forward without lateral movement. A triangle of skin can be excised from the base of the flap (Burow triangle) to aid in closure. An example is the V-Y advancement flap, which can be designed as a single pedicle or a bipedicle.
Advancement flap: The rectangular flap advances into a rectangular defect. The red triangular excisions are Burow triangles, which may be used to adjust the tension of closure.
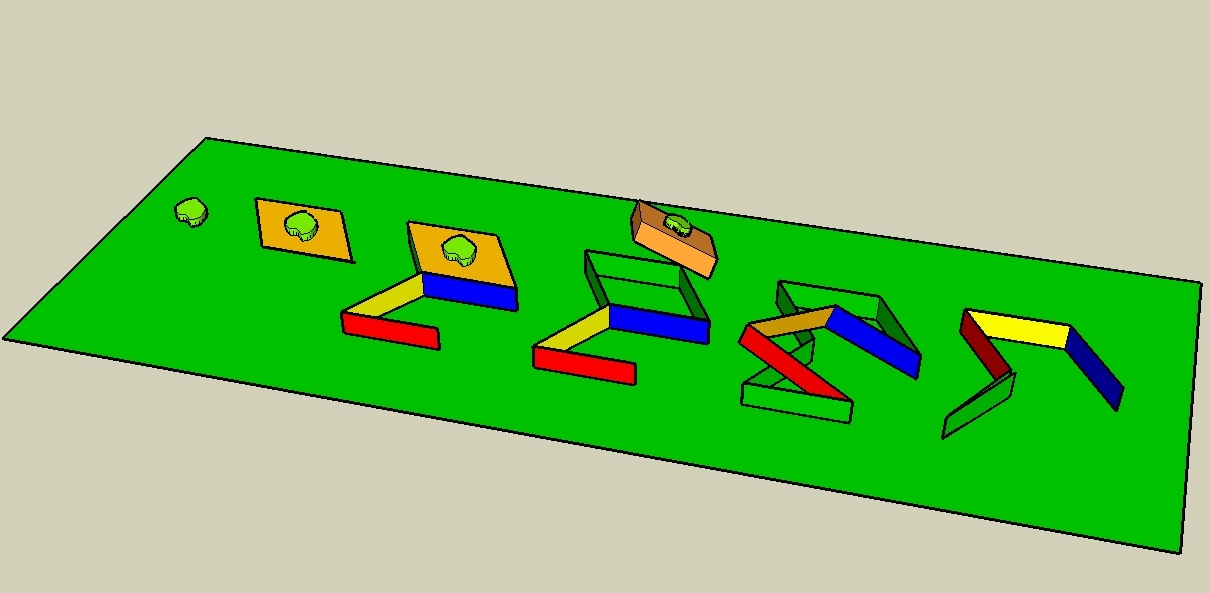
A rotation flap, shown below, is a semicircular flap that rotates about a pivot point into an adjacent defect. Design the arc as large as possible. The secondary defect or donor defect can be closed primarily or grafted. A backcut towards the pivot point along the diameter or a triangle of skin at the base (Burow triangle) may be added to assist in rotation and closure.
Rotational flap: The semicircular flap rotates into a triangular defect. The red triangular excision is a Burow triangle, which may be used to adjust the tension of closure.
A transposition flap moves laterally about a pivot point into an adjacent defect. Usually, it is designed as a rectangle. Design the flap to be longer than the defect, since transposition decreases the length. The donor site can be closed directly (occasionally facilitated by a backcut towards the pivot point) or closed with a skin graft or second skin flap. Examples of the transposition flap include the bilobed flap, the Z-plasty, and the Limberg (rhomboid) flap.
- The Z-plasty is a type of transposition flap in which two triangular flaps, designed with limbs of equal length, are interposed to exchange width and length. Classically, it is designed with 60° angles, which yield the maximum length.
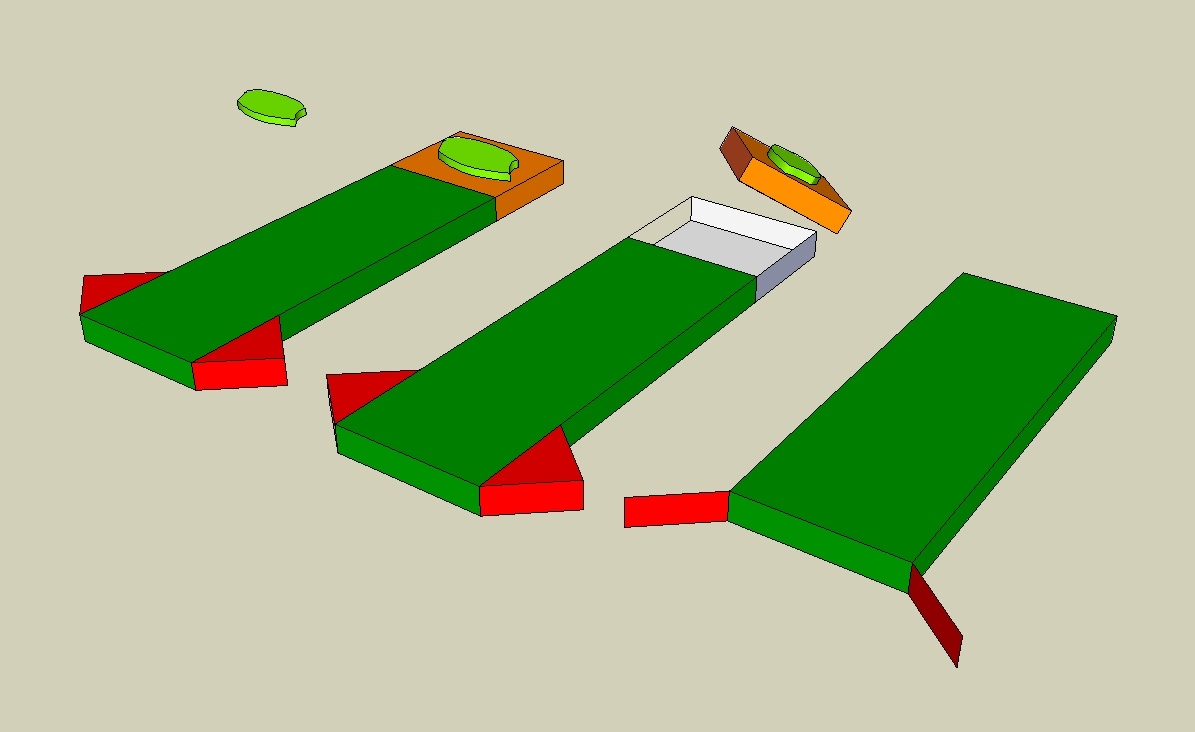
- The Limberg (rhomboid) flap, shown below, is designed in a rhomboid shape with 60° and 120° angles. Four flaps can be designed surrounding a rhomboid-shaped defect.7 The Dufourmentel flap is similar to a Limberg flap but the angles can vary up to 90°.8
The interpolation flap rotates about a pivot point into a nearby but not adjacent defect, with the pedicle passing above or below a skin bridge. An example is an island pedicle flap such as the Littler neurovascular flap for the hand.
One seldom-used flap type is the de-epithelialized turnover flap. In this flap design, an area of skin adjacent to a wound is de-epithelized. This dermis is raised as a flap, keeping a "hinge" area between the flap and the defect. The flap is turned over like a page in a book. As skin graft is applied to the underside of the dermis and the donor site.9,10
Distant flaps
Use distant flaps to cover nonadjacent defects. They may be transferred directly, tubed, or transferred by microvascular technique.
- Direct flap: A direct flap is transferred to a distant site directly so that the donor and recipient sites are approximated. The flap is divided after 1-3 weeks and inset. Examples of direct flaps include the groin flap (used for reconstruction of the hand) and the crossfinger or thenar flap (for fingertip reconstruction).
- Tubed flap: The tubed flap is transferred to a recipient site with the lateral flap edges sewn together, while the new blood supply is incorporated from the distant end of the flap. The tubed flap can be "waltzed" to another location by repeating the process. Sewing the edges together results in decreased risk of infection and contraction of the flap. An example of a tubed flap is a groin flap tubed and connected to the forearm, then divided and connected to the head and neck area for reconstruction.
- Microvascular flap: A microvascular free flap is a type of distant flap in which the flap, with its vascular pedicle, is divided completely from its donor vessels and anastomosed to the recipient vessels at the recipient site using a microsurgical technique. An example is the lateral thigh flap used in free-tissue transfer to the lower extremity for reconstruction.
Vascularity of Skin Flaps
The cutaneous vascular supply is composed of 3 main levels of vessels supplying the fascia, subcutaneous tissue, and skin. The subcutaneous vessels exit at the superficial fascia and divide the subcutaneous fat into a superficial and deep layer. It is formed by both musculocutaneous and septocutaneous arteries. The cutaneous or subdermal vessels are the main blood supply to the skin. Located at the junction between the deep reticular dermis and subcutaneous fat, they are responsible for the dermal bleeding from the edge of the skin flap. The dermal or subepidermal vessels are located at the papillary ridge to the dermal-epidermal junction. They undergo changes in size from arteries to arterioles to capillaries.11
A random skin flap lacks a specific named vessel. It is perfused from musculocutaneous or septocutaneous perforators located at the anatomic base of the flap. An example is a random local flap used in the reconstruction of a facial defect. An axial or arterial flap contains a direct cutaneous artery in the longitudinal axis of the flap within the subcutaneous fat. The vessels also can support a random portion of the skin. An example is the groin flap based on the superficial circumflex iliac artery.
Venous drainage from flaps occurs by way of the subcutaneous veins and/or venae comitantes of the supplying artery. The venous valves do not prevent retrograde flow from a distally based flap. This may be caused by incompetency secondary to denervation or by a reversal in pressure gradient across the valves and the opening of alternative channels that bypass the valves.
Microcirculation within flaps allows communication between the arterial and venous systems. Arterioles from the terminal vessels of the direct cutaneous, musculocutaneous, or septocutaneous systems run in the subcutaneous layer and then branch into the terminal arterioles supplying the subdermal plexus. The precapillary sphincter controls the blood flow into the capillary network; blood flows into the postcapillary venules and then into the collecting venules. Arteriovenous anastomoses or shunts are between the arterial and venous systems. Lymphatics also are involved in the microcirculation, and their disruption may contribute to flap edema.2
Principles of Flap Design
The donor site is the area from which the flap is raised, and the recipient site is the site to which the flap is inset. Prepare the recipient site properly prior to flap transfer. Then evaluate recipient site requirements. Address the requirements for color, texture, thickness, size, and any specialized function necessary to achieve the functional and cosmetic objectives. In choosing an appropriate donor site for coverage of the defect, consider donor site morbidity, complexity of the dissection, and durability. Also consider patient-related factors such as previous surgery in the area of the flap, trauma, radiation, and the patient's overall health status.
The vascularity of the flap must be understood for proper design and dissection. Design the flap to avoid tension on the pedicle, with careful attention to the relaxed skin tension lines, the elastic properties of the skin, and the flap's pivot point. The flap often is designed longer and wider than is expected to be necessary. The donor site can be closed primarily, with a skin graft, or with another skin flap.12
Flaps can be altered in numerous ways to fulfill certain requirements, including the following:
- Prefabrication of flaps allows transfer of a composite flap by incorporating cartilage or epithelial lining prior to transfer.13
- The Crane principle is a concept related to prefabrication. A flap is placed on a wound for a short period of time and then returned to its location, leaving behind a layer of tissue at the recipient site for a skin graft.11
- Flaps may be expanded by the placement of tissue expanders beneath them to create larger donor sites and increase survival length.14
- Delaying the flap also can increase the length that can be successfully transferred. In this process, raise the flap in 2 stages instead of 1, allowing approximately 7-14 d between the 2 procedures. Dissect or divide the flap partially, leaving some blood supply intact, and leave it in its native bed. Theories explaining the delay phenomenon include vasodilation caused by the sympathectomy and a hyperadrenergic state lasting 18-36 h after a flap is raised. However, this period of vasoconstriction does not occur at the second stage. Delaying a flap improves its vascularity and preconditions the flap to ischemia.15
Monitoring of Skin Flaps
After successful flap design and implementation, monitor the flap for viability as early recognition of ischemia is important in preventing subsequent flap necrosis, thus flap failure. Clinical observation is the best method to assess a flap. An extremely pale flap may signify arterial insufficiency, while a blue flap may be secondary to a failure of venous outflow. Two additional tests often used to assess viability are capillary refill and warmth. Assessment of bleeding from the flap after stabbing it with a small needle is believed to be one of the most reliable methods of clinical assessment.16
In addition to clinical assessment, objective tests such as pH monitoring and transcutaneous oxygen tension (PO2)17,18 can aid in early detection of flap ischemia.19 Doppler ultrasound is used commonly,20 and laser Doppler is increasingly useful.21 Surface temperature monitoring is another dependable technique.22 Fluorescein dye and illumination with a Wood lamp is useful; however, it is cumbersome, and adverse reactions to the dye have been reported.23,24
Complications of Flaps
Multiple factors contribute to flap failure.
Preoperative causes
Poor flap design is one of the most common causes of flap failure. Inadequate flap size, violation of the blood supply to the flap, or design of the flap in radiated or traumatized tissue often causes early problems in the surgical procedure. Additionally, patient-related factors such as smoking, hypertension, and poor overall health can contribute to flap complications.12
Intraoperative causes
Technical errors such as injuring the blood supply during dissection, creating too much tension on the flap, or twisting or kinking the flap pedicle can cause flap ischemia and necrosis.
Postoperative causes
Hematoma can cause pressure on the flap and lead to necrosis. Infection also can cause partial or complete flap necrosis. The donor site is another potential source of complications (eg, significant scarring, wound dehiscence, poor skin graft acceptance if the wound was grafted).
Multimedia
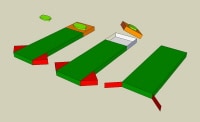 | Media file 1: Advancement flap: The rectangular flap advances into a rectangular defect. The red triangular excisions are Burow triangles, which may be used to adjust the tension of closure. |
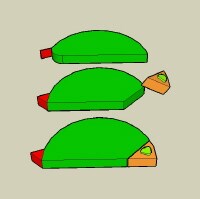 | Media file 2: Rotational flap: The semicircular flap rotates into a triangular defect. The red triangular excision is a Burow triangle, which may be used to adjust the tension of closure. |
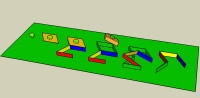 | Media file 3: The Limberg flap: This is a transposition flap, showing closure of a rhomboid-shaped defect. |
Keywords
skin flap, random skin flap, skin grafts, skin grafting, graft survival, skin flaps, graft, flap, random flap, wound coverage, flap classification, wound coverage, wound bed, blood supply, flap blood supply, flap vascularity, local flap, advancement flap, rotation flap, transposition flap, Z-plasty, Limberg flap, rhomboid flap, interpolation flap, turnover flap, Littler flap, distant flap, direct flap, tubed flap, microvascular flap, skin flap vascularity, flap design, flap closure, skin flap design, skin flap closure, skin flap complications, flap prefabrication, prefab flap, Crane principle, tissue expander, recipient site, flap delay, flap tension
The authors and editors of eMedicine gratefully acknowledge the contributions of previous author Kerri M Woodberry, MD, to the development and writing of this article.

Không có nhận xét nào:
Đăng nhận xét