Introduction
Background
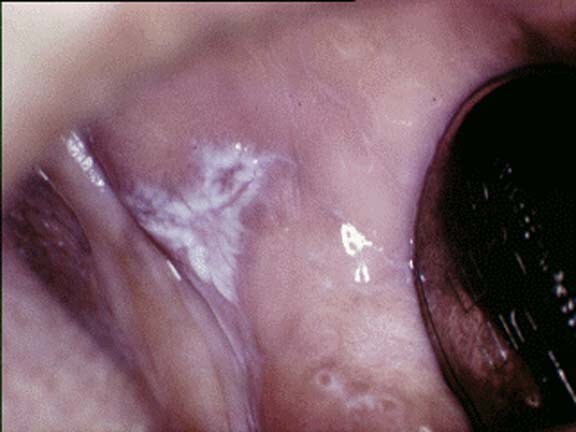
Oral lichen planus (OLP) is a chronic inflammatory disease that causes bilateral white striations, papules, or plaques on the buccal mucosa, tongue, and gingivae. Erythema, erosions, and blisters may or may not be present.
Pathophysiology
Current data suggest that oral lichen planus is a T-cell–mediated autoimmune disease in which autocytotoxic CD8+ T cells trigger apoptosis of oral epithelial cells.1,2
The dense sub-epithelial mononuclear infiltrate in oral lichen planus is composed of T cells and macrophages, and there are increased numbers of intra-epithelial T cells. Most T cells in the epithelium and adjacent to the damaged basal keratinocytes are activated CD8+ lymphocytes. Therefore, early in the formation of oral lichen planus lesions, CD8+ T cells may recognize an antigen associated with the major histocompatibility complex (MHC) class I on keratinocytes. After antigen recognition and activation, CD8+ cytotoxic T cells may trigger keratinocyte apoptosis. Activated CD8+ T cells (and possibly keratinocytes) may release cytokines that attract additional lymphocytes into the developing lesion.2
Oral lichen planus lesions contain increased levels of the cytokine tumor necrosis factor (TNF)–alpha.3,4 Basal keratinocytes and T cells in the subepithelial infiltrate express TNF in situ.5,6 Keratinocytes and lymphocytes in cutaneous lichen planus express elevated levels of the p55 TNF receptor, TNF-RI.7 T cells in oral lichen planus contain mRNA for TNF and secrete TNF in vitro.8 Serum and salivary TNF levels are elevated in oral lichen planus patients.9,10,11,12 TNF polymorphisms have been identified in patients with oral lichen planus, and they may contribute to the development of additional cutaneous lesions.13 Oral lichen planus has been treated successfully with thalidomide,14,15 , while thalidomide is known to suppress TNF production.16,17 Together, these data implicate TNF in the pathogenesis of oral lichen planus.
The lichen planus antigen is unknown, although it may be a self-peptide (or altered self-peptide), in which case lichen planus would be a true autoimmune disease. The role of autoimmunity in the pathogenesis is supported by many autoimmune features of oral lichen planus, including its chronicity, onset in adults, predilection for females, association with other autoimmune diseases, occasional tissue-type associations, depressed immune suppressor activity in patients with oral lichen planus, and the presence of autocytotoxic T-cell clones in lichen planus lesions. The expression or unmasking of the lichen planus antigen may be induced by drugs (lichenoid drug reaction), contact allergens in dental restorative materials or toothpastes (contact hypersensitivity reaction), mechanical trauma (Koebner phenomenon), viral infection, or other unidentified agents.18,19,20
Frequency
United States
The prevalence of oral lichen planus in the United States is unknown.
International
Oral lichen planus affects approximately 1-2% of the general adult population, although the prevalence of the disease is unknown in many areas.21 Oral lichen planus is a common noninfectious oral mucosal disorder among adult patients who attend oral pathology and oral medicine clinics.
Mortality/Morbidity
- Oral squamous cell carcinoma (SCC) developed in fewer than 5% of patients with oral lichen planus who did not use tobacco (see Complications).22,23,24 Also see Cancers of the Oral Muscosa.
- Patients with atrophic (erythematous) or erosive (ulcerative) disease commonly have significant local morbidity.
Race
Oral lichen planus affects all racial groups.
Sex
The female-to-male ratio for oral lichen planus is 1.4:1.
Age
Oral lichen planus predominantly occurs in adults older than 40 years, although younger adults and children can be affected.
Clinical
History
The clinical history of oral lichen planus and oral lichenoid lesions varies. Complete history taking and physical examination by a dermatologist may be required in patients with extra-oral symptoms or signs associated with oral lichen planus.25
Lichen planus may arise in patients with other immunologically mediated disorders, including alopecia areata, dermatomyositis, lichen sclerosis et atrophicus, morphea, myasthenia gravis, primary biliary cirrhosis, ulcerative colitis, and vitiligo.
- In many patients, the onset of oral lichen planus is insidious, and patients are unaware of their oral condition. In such instances, the referring medical or dental practitioner identifies the clinical changes in the oral mucosa.
- Some patients report a roughness of the lining of the mouth, sensitivity of the oral mucosa to hot or spicy foods or oral hygiene products, painful oral mucosa, sore gums, red or white patches on the oral mucosa, red gums, or oral ulcerations.
- Approximately two thirds of patients with oral lichen planus report oral discomfort, especially in association with atrophic and erosive lesions.
- Erythematous and erosive lesions are often sensitive or painful.
- Symptoms vary from mucosal sensitivity to continuous debilitating pain.
- Oral mucosal lichenoid lesions may occur after the administration of systemic drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), sulfonylureas, antimalarials, beta-blockers, and some angiotensin-converting enzyme (ACE) inhibitors. The period between the commencement of the drug therapy and the clinical appearance of oral lichen planus–like disease varies.
- In rare cases, oral mucosal lichenoid lesions occur after a dental restoration is performed or after the patient starts using a denture; the lag period varies. Patients with an associated allergy to metals or components of the appliance should be evaluated by means of patch testing.26
- Up to 44% of patients with oral lichen planus develop coincident skin lesions. Conversely, more that 70% of patients with cutaneous lichen planus develop coincident oral lichen planus.
- The genitals are involved in as many as 25% of women with oral lichen planus, compared with only 2-4% of men with oral lichen planus.
- The features are similar to those of the oral lesions.
- Patients do not often complain of pain or pruritus, although on questioning, they may admit to such symptoms.
- In patients with oral lichen planus, scalp involvement (lichen planopilaris) is rare.
- Nail involvement in patients with oral lichen planus is uncommon.
- In a small group of patients, lichen planus may involve the esophagus.
Physical
Pertinent physical findings in oral lichen planus are limited to the oral mucosa. Some patients present with coincident lesions on the skin, scalp, nails, genital mucosa, esophageal mucosa, larynx, and conjunctivae. Complete history taking and physical examination by a dermatologist may be required in patients with extra-oral symptoms or signs associated with oral lichen planus.25
Patients with reticular lesions are often asymptomatic, whereas those with atrophic (erythematous) or erosive (ulcerative) disease commonly have significant local morbidity. The oral pain is variable and exacerbated by trauma and foods, particularly those that are hot, spicy, or acidic.
- Oral mucosal lesions are variable and present as white striations (Wickham striae), white papules, white plaques, erythema (mucosal atrophy), erosions (shallow ulcers), or blisters.
- The lesions predominantly affect the buccal mucosa, tongue, and gingivae, although other oral sites are occasionally involved.
- The lesions are usually bilateral.
- The lesions may appear as a mixture of clinical subtypes. For example, white streaks and gray streaks may form a linear or reticular pattern on an erythematous background. Alternatively, a central area of shallow ulceration (erosion) may have a yellowish surface (fibrinous exudate) surrounded by an area of erythema.
- In most patients, telltale white striations or papules are evident on the buccal mucosa or on the lateral margin of the tongue, either alone or in combination with other lesions.
- Gingival lesions commonly appear with a fiery red erythema that affects the entire width of the attached gingiva, a condition previously called desquamative gingivitis.
- In patients predisposed to pigmentation, oral lichen planus lesions may be associated with patchy brown melanin deposits in the oral mucosa (inflammatory melanosis).
- Oral lichen planus lesions usually persist for many years with periods of exacerbation and quiescence.
- During periods of exacerbation, the area of erythema or erosion increases, with increased pain and sensitivity.
- During periods of quiescence, the area of erythema or erosion decreases, with decreased pain and sensitivity. Patients are often unaware of quiescent oral lichen planus, which may manifest as faint white striations, papules, or plaques.
- Exacerbations of oral lichen planus have been linked to periods of psychological stress and anxiety.
- Lichenoid drug reactions have the same clinical features as those of idiopathic oral lichen planus.
- Lichenoid disease may be unilateral and associated with circulating epithelial antinuclear antibodies, but few data support this possibility.
- Rarely, lichenoid reactions of the oral mucosa occur on the oral mucosa in contact with (or close to) an amalgam or composite resin dental restoration, or a denture component.
- Mechanical trauma (the Koebner phenomenon) may exacerbate lichenoid lesions, especially when it affects the midline of the buccal mucosa or the lateral margin of the tongue.
- Up to 44% of patients with oral lichen planus develop coincident skin lesions. These typically appear as pruritic, flat-topped, violaceous papules and plaques that predominantly affect the flexor aspects of the wrists or ankles, the extensor aspects of the lower legs, the skin of the lower central part of the back, and the natal cleft.
- The genitals are involved in as many as 25% of women with oral lichen planus, compared with only 2-4% of men with oral lichen planus. The features are similar to those of oral lesions.
- Nail involvement causes pitting, subungual hyperkeratosis, longitudinal melanonychia, onychorrhexis (longitudinal ridging and grooving), onychoschizia (distal splitting), and onycholysis (separation of the nail plate from the nail bed). Permanent damage to the nail matrix results in the formation of a pterygium (raised central ridge) and permanent nail loss (anonychia).
- Scalp involvement (lichen planopilaris) causes follicular and perifollicular violaceous scaly pruritic papules, follicular plugging, bottlebrush hair formation (multiple hair shafts emerging from a single follicular orifice), and atrophic scarring with permanent patchy hair loss.
- Rarely, laryngeal, esophageal, and conjunctival involvement occur.
Causes
Current data suggest that oral lichen planus is a T-cell–mediated autoimmune disease in which autocytotoxic CD8+ T cells trigger the apoptosis of oral epithelial cells. However, the precise cause of oral lichen planus is unknown.
Reported associations between oral lichen planus and systemic diseases may be coincidental, because (1) oral lichen planus is relatively common, (2) oral lichen planus occurs predominantly in older adults, and (3) many drugs used in the treatment of systemic diseases trigger the development of oral lichenoid lesions as an adverse effect.
In many patients, a cause for the oral lichenoid lesions cannot be identified; in these patients, the disease is called idiopathic oral lichen planus.
- Oral lichenoid drug reactions may be triggered by systemic drugs including NSAIDs, beta-blockers, sulfonylureas, some ACE inhibitors, and some antimalarials. In patients with oral lichenoid lesions, be alert for any systemic drug as a cause.
- Oral lichenoid contact-sensitivity reactions may be triggered by contact allergens including dental amalgam composite resin, and toothpaste flavorings, especially cinnamates. Skin patch testing may help in identifying contact allergens (see Other Tests). If an allergy is detected, lesions may heal when the offending material is removed.
- Oral lichenoid lesions may be triggered by mechanical trauma (Koebner phenomenon) due to calculus deposits, sharp teeth, rough surfaces of dental restorations or prostheses, cheek or tongue biting, and oral surgical procedures. Scale any teeth associated with oral lichen planus lesions to remove calculus deposits and reduce sharp edges. Dental restorations and prostheses that are associated with oral lichen planus lesions should be mirror-polished.
- Some studies have revealed viral infections in oral lichen planus, including those due to human papillomavirus (HPV-6, 11, 16, or 18) and human herpesvirus 6. A causal role for viral infection in oral lichen planus has not been identified.
- Some studies show an increased incidence of C albicans infection in oral lichen planus. A causal role for C albicans infection in oral lichen planus has not been identified.
- Some study findings suggest an association between oral lichen planus and chronic hepatic diseases such as hepatitis C virus (HCV) infection, autoimmune chronic active hepatitis, and primary biliary cirrhosis.27,28
- This association probably reflects the geographic distribution of HCV disease and lichenoid reactions to various drug therapies (eg, interferon alpha for HCV disease, penicillamine for primary biliary cirrhosis).
- Oral lichen planus is associated with HCV infection and liver disease in parts of Japan and southern Europe. An association between oral lichen planus and HCV infection has not been detected in British, French, German, Scandinavian, or American patients.
- Oral lichenoid lesions may arise in people who habitually chew betel quid. A causal role for betel quid in oral lichen planus has not been identified.
- Oral lichenoid lesions are part of the spectrum of chronic graft-versus-host disease that occurs after allogeneic hemopoietic stem cell transplantation.
- No consistent association with human leukocyte antigen (HLA) is reported in oral lichen planus. This finding suggests that the patient's genetic background does not play a critical role in oral lichen planus pathogenesis.
- Exacerbations of oral lichen planus have been linked to periods of psychological stress and anxiety.
- Little evidence supports a connection between diabetes mellitus and oral lichen planus. The oral lichenoid lesion in Grinspan syndrome (triad of oral lichen planus, diabetes mellitus, and hypertension) is probably an adverse effect of the drug therapy for diabetes mellitus and hypertension.






very good post thanks a lot
Trả lờiXóaTOSHIBA PLT-805AT
There are 5 Home Remedies of Lichen Planus Treatment. Cool Compress, Aloe Vera, Turmeric, Oats and Ginger. These home remedies are very effective and recover lichen planus successfully without any side effects.
Trả lờiXóaVarious Lichen Planus Home Remedies Treatment can cure the skin disease. Herbs Solutions By Nature are offering Lichreton, an Herbal Supplements made out of 100% natural ingredients. It is a powerful combination of carefully chosen potent herbs that have no side effects. It is totally natural and free of synthetic chemicals.
Trả lờiXóahttp://www.herbs-solutions-by-nature.com/Lichen-Planus.php
Lichen Planus on the skin results in few bumps which are purplish in shading and flat topped. Very often, Lichen Planus Home Remedies for this issue is gone for controlling the causes and triggers. You could also try Lichen Planus Herbal Treatment for treating the discomfort caused by the condition.
Trả lờiXóahttp://www.herbs-solutions-by-nature.com/Lichen-Planus.php
Lichen Planus on the skin results in few bumps which are purplish in shading and flat topped. Very often, Lichen Planus Home Remedies for this issue is gone for controlling the causes and triggers. You could also try Lichen Planus Herbal Treatment for treating the discomfort caused by the condition.
Trả lờiXóahttp://www.herbs-solutions-by-nature.com/Lichen-Planus.php
UV treatment and antihistamine medications are treatment choices that are generally started. Lichen Planus Herbal Remedies that have characteristic mixes which can give help from hypersensitivity and therefore oversee lichen planus are said in the blog below.... http://www.naturalherbsclinic.com/Lichen-Planus.php
Trả lờiXóaThanks for sharing this helpful post....!
Trả lờiXóahttp://www.herbs-solutions-by-nature.com/Lichen-Planus.php
Trả lờiXóaLichen planus are rashes on the skin or inside of the mouth are symptoms of lichen planus. The aim of Lichen Planus Herbal Treatment is to reduce symptoms and healing rashes with proper diagnosis.
https://www.herbs-solutions-by-nature.com/Lichen-Planus.php
http://b4tea.blogspot.com/2012/08/lichen-planus-scar-lifestyle-and-home.html
Trả lờiXóaHerbal Treatment for Lichen Planus learns about the Symptoms, Causes and Diagnosis.Natural Herbal Treatment for Lichen Planus with Herbal Product Lichreton Natural Supplement for inflammatory condition marked by an itchy, bumpy, pink or purple rash skin.
Trả lờiXóaAloe Vera can do wonders for health and so is Lichen Planus Herbal Treatment . Local application of Aloe Vera extract can soothe your skin and help get you rid of those ugly looking pigmented patches.
Trả lờiXóaI was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóaNhận xét này đã bị tác giả xóa.
Trả lờiXóaI Strongly recommend Dr.uwenboherbalhome@gmail.com to everyone here. After been diagonised with HS, I finally got cured of this illness through natural herbs. It unbelievable after spending much on medications which came with high side effect. It an amazing miracle in my life and wishes to pass it to anyonoe suffering and needs help..Reach him on whatsapp +2349052309005 for permanent healing.You can aslso search his youtube channel on Dr.uwenboherbalhome for assistance..He is also specialised in curing HSV 1&2, SKIN INFECTION/DISEASE, LICHEN PLANUS, SKIN WARTS, GERNITAL WARTS, HPV, TMAU, BAD BREATH e.t.c.
Trả lờiXóaWe are really grateful for your blog post. You will find a lot of approaches after visiting your post. I was exactly searching for. Thanks for such post and please keep it up. Great work.
Trả lờiXóaRegards,
Lichen planus pigmentosus specialist
Treating Lichen Planus with cold-pressed oil, oats, ginger are one of the best ways and it can turn out to be really helpful for you. Did you know that Lichen Planus can also be treated with the help of homeopathic medicine. Afecto Homeopathy Clinic is one of the best Homeopathic Clinic in India as it will do its best to treat Lichen Planus.
Trả lờiXóa