Odontogenesis
Odontogenic tumors represent the results of interruptions in or reactivation of tissues involved in the normal sequence of odontogenesis. The nature of the neoplasm is determined by the stage of development at which the arrest occurs. A brief review of odontogenesis is helpful in understanding the pathogenesis and behaviors of odontogenic tumors.
At the sixth week of gestation, odontogenesis begins with proliferation of certain areas of oral ectoderm to form the dental lamina. At each of the locations where a tooth will be formed, a downgrowth from the dental lamina forms the beginning of the enamel organ. Together, the enamel organ, dental papilla, and dental sac are the formative structures for the entire tooth and supporting structures. The dental lamina, which originally connected the enamel organ to the oral epithelium, breaks up, thus separating the developing tooth bud from the epithelium of the oral cavity.
Each stage in the development of the tooth is associated with certain events that are summarized below. Interruptions in this sequence may lead to the formation of odontogenic tumors.
- Bud stage: Initiation and formation of the enamel organ occurs.
- Cap stage: Proliferation occurs. Unequal growth leads to the characteristic shape. The peripheral cells are cuboidal and are termed the outer enamel epithelium (OEE), and the cells in the concavity are tall columnar cells termed the inner dental epithelium. At the same time, polygonal cells between outer and inner enamel epithelia begin to separate and form the delicate cellular network known as the stellate reticulum (SR), the spaces of which are filled with a mucoid fluid. Histologically, this material resembles Wharton jelly. The proliferation of the epithelial components just discussed leads to condensation of the enclosed ectomesenchyme and formation of the dental papilla. The cells of the dental papilla eventually form tooth pulp and dentin. Similarly, condensation of the ectomesenchyme surrounding the enamel organ leads to creation of the dental sac. The cells of the dental sac eventually form cementum and the periodontal ligament.
- Bell stage: Histodifferentiation (early) and morphodifferentiation (late) occur. The enamel organ now assumes an elongated bell shape and has 4 distinct types of epithelial cells: inner enamel epithelium (IEE), stratum intermedium, SR, and OEE.
- The IEE organizes and induces the adjacent cells of the dental papilla to differentiate into odontoblasts, which form dentin. The dentin, in turn, induces the IEE to differentiate into ameloblasts, which lay down enamel matrix opposite the dentin. This reciprocal induction is essential for the formation of the tooth.
- The stratum intermedium consists of a few layers of squamous cells between the IEE and the SR. This layer is apparently essential to enamel formation because it is absent in the part of the tooth germ that outlines areas of the tooth without enamel.
- The SR expands by increasing the amount of intracellular fluid. It collapses before the formation of enamel, leaving the ameloblasts closer to the nutrient capillaries adjacent to the OEE.
- The OEE, which was formerly smooth, becomes folded. In the folds, the adjacent mesenchyme of the dental sac forms papillae with capillary loops to provide a supply of nutrients for the metabolic activity of the avascular enamel organ. The enamel organ also forms Hertwig epithelial root sheath, which determines the shape of the roots and initiates the formation of dentin in the roots.
- Apposition: The deposition of the matrix of the hard dental structures occurs next. These structures then begin calcification, eruption, and, with time, attrition.
Odontogenic Tumors
Ameloblastoma
Ameloblastoma (see Images 1-3) is an entirely epithelial tumor arising from the dental lamina, Hertwig sheath, the enamel organ, or the lining of dental follicles/dentigerous cysts. Ameloblastoma is the most common epithelial odontogenic tumor. Ameloblastomas usually occur in individuals aged 20-40 years; however, the unicystic variant (see Surgical considerations, below) most often occurs in adolescents. This lesion occurs in both the maxilla and mandible, but the posterior mandible is the most common location; only 20% of lesions are found in the maxilla. The lesion is distributed equally between males and females.
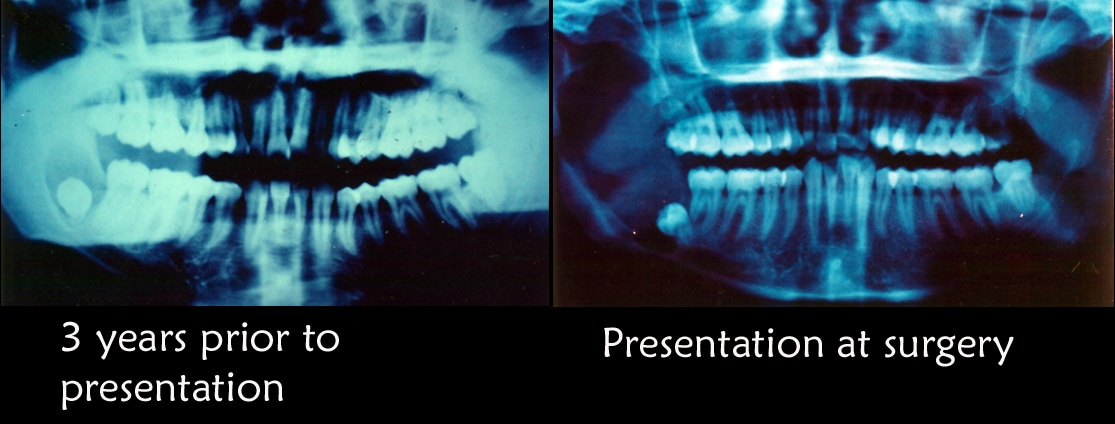
Initial radiographic appearance. The patient was advised that biopsy of cystic lesion was indicated; however, he did not schedule an appointment because he was planning to leave the country. He did not follow up for 3 years. He returned to the United States and sought care from a general dentist when he noted some mild facial swelling and discomfort. He was referred to the oral and maxillofacial surgery (OMFS) clinic. The second radiograph depicts the appearance of the lesion at the second presentation.
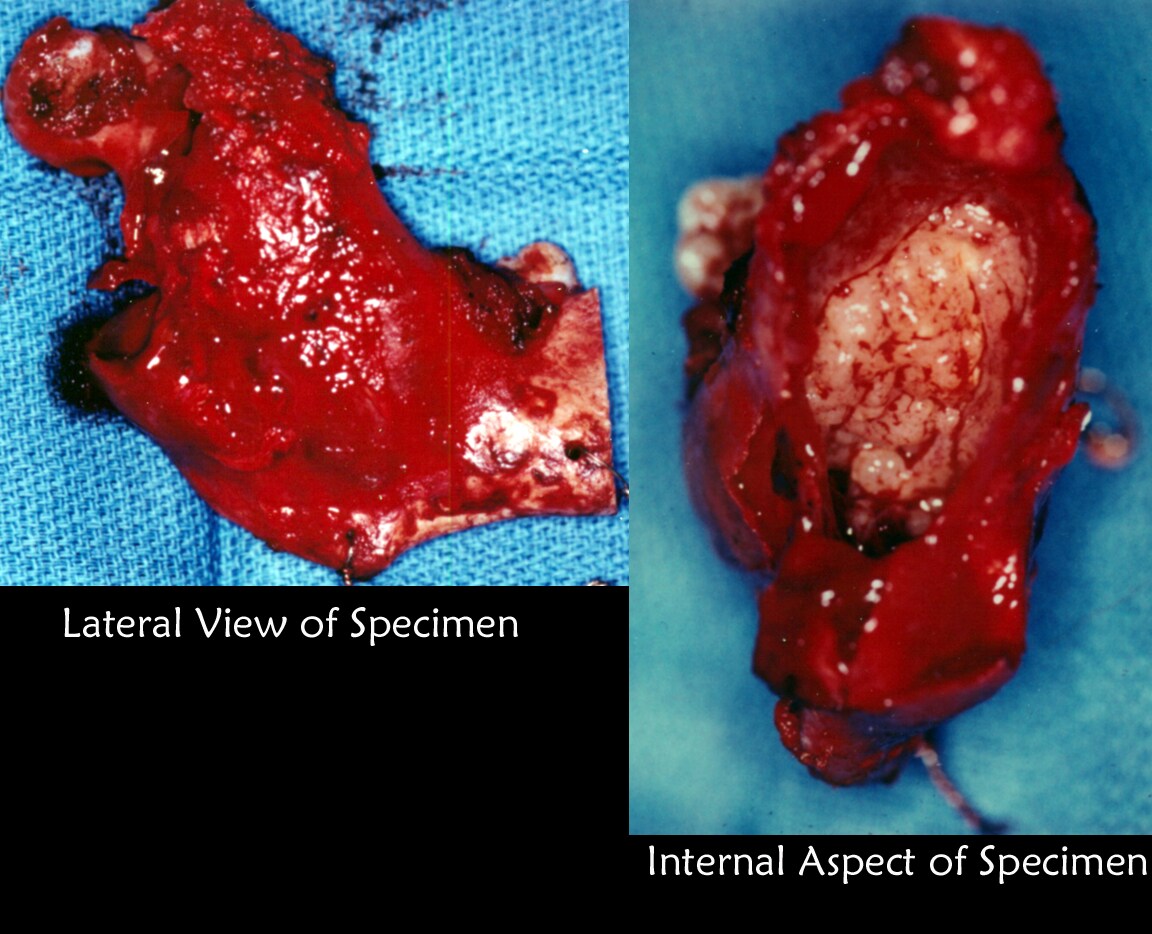
The patient was advised that biopsy of cystic lesion was indicated; however, he did not schedule an appointment because he was planning to leave the country. He did not follow up for 3 years. He returned to the United States and sought care from a general dentist when he noted some mild facial swelling and discomfort. He was referred to the oral and maxillofacial surgery (OMFS) clinic. Incisional biopsy revealed the lesion to be an ameloblastoma. Treatment consisted of segmental resection of the entire mandible from the condyle to the area of the second premolar. The lateral and internal aspects of the resected specimen are depicted.
The patient was advised that biopsy of cystic lesion was indicated; however, he did not schedule an appointment because he was planning to leave the country. He did not follow-up for 3 years. He returned to the United States and sought care from a general dentist when he noted some mild facial swelling and discomfort. He was referred to the oral and maxillofacial surgery (OMFS) clinic. Incisional biopsy revealed the lesion to be an ameloblastoma. Treatment consisted of segmental resection of the entire mandible from the condyle to the area of the second premolar. The defect was reconstructed using autogenous rib, iliac crest, and tibial bone. Note the stable occlusion and excellent function obtained.
Although ameloblastoma generally is not classified as a malignant lesion (a rare malignant variant exists), it is extremely aggressive and infiltrative. Many have suggested that this lesion should be considered a low-grade or indolent malignancy, similar to basal cell carcinoma. Many histologic and behavioral similarities are found between the 2 lesions. It generally does not metastasize but is slow growing, persistent, and hard to eradicate. If ameloblastoma is not noticed as an incidental finding on radiographs taken for other purposes, the first symptom is usually painless bony expansion.
Radiographic findings
Ameloblastomas typically appear as an expansile multilocular radiolucency in the area of the lower third molar, but they may be found anywhere in the jaws (see Image 1). These lesions may be unilocular when small, and they often resorb the teeth they contact. These lesions are never radiopaque.
Histologic characteristics
Ameloblastoma does not have a capsule. The neoplastic component is purely epithelial and resembles the cap stage of odontogenesis (ie, polarized tall columnar cells on the outer aspect of the lesion with SR on the inner aspect, which may form a cyst). The lesion may have a reactive connective tissue component that is not neoplastic. This is a nonfunctional tumor, ie, it does not induce the surrounding connective tissue, which in turn is unable to induce enamel formation. In effect, these tumors represent arrested odontogenesis. Multiple histologic varieties exist, eg, the acanthomatous type in which the SR is replaced by squamous cells and pearls, the granular cell type in which the SR is replaced by granular cells, and the plexiform type in which the SR is reduced or absent.
Treatment
The treatment of ameloblastoma is surgical excision with wide free margins (see Surgical considerations, below). Appropriate reconstruction may be performed at the same time. All patients with ameloblastoma, regardless of surgical treatment method or histologic type, must be monitored radiographically throughout their lifetime. If excision is inadequate, recurrence is common.
Surgical considerations- The maxillary ameloblastoma is not confined by the strong cortical plate found in the mandible. In addition, the posterior maxilla lies in close relationship to many vital structures. These factors make strong arguments for aggressive and definitive surgical treatment of the maxillary ameloblastoma.
- In the mandible, 1-cm clear margins are considered the standard. This may be accomplished with block or segmental resection, depending on the relationship of the lesion to the inferior cortical border.
- The single exception to this may be the unicystic ameloblastoma. This variant most commonly appears in late adolescence and, as the name suggests, is characterized by a unicystic radiolucency that most commonly is found in the area of the mandibular third molars. Unlike other types of ameloblastomas, it is believed that this lesion is encapsulated and can be removed with enucleation/curettage procedures alone. These lesions may recur, and recurrences may require more aggressive treatment. Most authors believe that if left untreated, this lesion becomes an ameloblastoma of one of the classic varieties, leading to the corollary conclusion that these lesions simply represent an early stage in the development of ameloblastoma.
- For peripheral ameloblastoma, a more conservative excision with close clinical follow-up is the standard of care.
- Basal cell carcinoma: Basal cell carcinoma is another infiltrative, essentially nonmetastasizing adnexal neoplasm. Basal cell carcinomas and ameloblastomas are slow growing but persistent, and they may cause death via local extension into vital structures. If one considers that the tooth is an oral adnexal structure, then it is easy to understand why ameloblastoma may be seen as an analogue to basal cell carcinoma.
- Tibial adamantinoma: This lesion is histologically similar to the plexiform variety of ameloblastoma. It is considered a low-grade malignancy and, as the name suggests, is found in the tibia.
- Craniopharyngioma: This pituitary tumor arises from Rathke pouch, part of the oral stomadeum that histologically appears somewhat like ameloblastoma. However, it is actually more like the Gorlin cyst.
- Peripheral ameloblastoma: This lesion is histologically identical to the central ameloblastoma, but it does not involve bone and is confined entirely to the gingiva. It has a lower potential for growth and invasion than the central ameloblastoma, and, quite possibly, it is responsible for reported cases of basal cell carcinoma in the gingiva.
- Malignant ameloblastoma: Approximately 2% of ameloblastomas metastasize, usually to the lungs. These lesions may actually be the result of aspiration of material from fungating lesions in the oral cavity and, therefore, do not represent true metastases.
- Ameloblastic carcinoma: These are cytologically malignant lesions with hyperchromatism, pleomorphism, and high mitotic activity. Real metastases occur with ameloblastic carcinoma.
Adenomatoid Odontogenic Tumor
The adenomatoid odontogenic tumor (AOT) is a fairly uncommon tumor, but it usually can be easily identified from its clinical and radiographic appearance. It often is remembered as the "two-thirds tumor." It most commonly occurs in the second and third decades of life (12-20 y). Two thirds of the cases occur in the anterior maxilla, one third occur in the anterior mandible, and it is never found posterior to the premolars. Two thirds of the cases occur in females, and two thirds of the cases are associated with an impacted tooth (usually the cuspid).
This tumor originates from the reduced enamel epithelium of the dental follicle and histologically reproduces the IEE. It is generally asymptomatic but may present with mild swelling or in association with a clinically missing tooth.
Radiographic findings
This lesion generally appears as a well-demarcated radiolucency. In 75% of cases, it is associated with an unerupted tooth, usually the canine. It may contain radiopaque flecks, which represent calcified material. If associated with a tooth, it generally attaches to the tooth further apical on the root than the typical dentigerous cyst.
Histologic characteristics
Technically, this is a hamartoma rather than a true neoplasm because it has a limited growth potential. It has a thick fibrous capsule filled with a proliferation of epithelial elements that form nodules and ductlike structures (eg, organoid nodules of cuboidal or low columnar cells separated by spindly epithelium). In the absence of connective tissue to induce the formation of enamel, the product of these cells, a pre-enamel matrix, is thought to degenerate and ultimately leave areas of dystrophic calcification and amyloid.
Treatment
The recommended treatment of these lesions is simple removal. If left alone, these structures probably involute. However, they can become quite large. Most are removed at biopsy. If AOT is incompletely removed at biopsy, the literature suggests that the remainder of the lesion degenerates. They are not known to recur.
Calcifying Epithelial Odontogenic Tumor
The calcifying epithelial odontogenic tumor (CEOT), or Pindborg tumor, is a benign infiltrative odontogenic tumor that is one of the rarest. It is named after Jens Pindborg, the Danish oral pathologist. It is most often found in the mandibular molar/premolar region, but 33% of cases are found in the maxilla. It is associated with an unerupted or impacted tooth in 50% of cases. CEOT is an infiltrative neoplasm and causes destruction with local expansion. It is derived from the stratum intermedium and has a lower growth potential than ameloblastoma. Not surprisingly, it is less aggressive than ameloblastoma.
Radiographic findings
These lesions can be radiolucent, but they more characteristically are mixed lucent and opaque masses, exhibiting a snow-driven appearance.
Histologic characteristics
The histologic view of this lesion is worrisome because it appears as invasive infiltrative islands in bone. These islands look like pure squamous cells with a high degree of nuclear pleomorphism; however, Liesegang rings (ovoid dystrophic calcifications), a normal mature cytoplasm (large polyhedral cells with good intercellular bridges and filled with mature keratin granules), and the lack of mitotic figures help to distinguish this lesion from squamous cell carcinoma. The pleomorphism noted is secondary to degeneration of the nuclei and necrobiosis, and dystrophic calcification and amyloid conversion are characteristic in dying epithelial cells.
Treatment
The treatment of this lesion is complete surgical excision. The recurrence rate for CEOT is 4%. The lesion is slow growing and requires long-term follow-up monitoring for recurrence (at least 5-10 y). No cases of malignant transformation are reported.
Keratinizing and Calcifying Odontogenic Cyst
The keratinizing and calcifying odontogenic cyst (KCOC), or Gorlin cyst, is not actually a cyst but rather a neoplasm with cystic tendencies. Some KCOC lesions are actually solid. This is a very rare lesion with no age, sex, or location predilections. KCOC may be found anywhere in the jaws, and one fourth of lesions are found in peripheral soft tissue (eg, gingiva). If KCOC is not discovered as an incidental finding on radiographic examination, the earliest clinical presentation usually is a localized swelling.
These lesions arise from a more mature enamel epithelium than ameloblastoma, and, accordingly, they have less growth potential.
Radiographic findings
These are nondescript radiolucencies that may contain flecks of opacity. They may become quite large if not discovered serendipitously.
Histologic characteristics
These lesions are lined by an epithelium that is similar in appearance to ameloblastoma (eg, polarized basal layer and SR are present). KCOC appears somewhat similar to the unicystic ameloblastoma, with masses of keratinized squamous epithelial cells within the SR. However, these cells have no nuclei and are called ghost cells. This ghost epithelium eventually herniates into the connective tissue, causing a connective tissue foreign body response that results in dentinoid dystrophic calcification and the formation of granulation tissue. More simply, this lesion represents enamel epithelium that has a tendency to mature but is unable to form enamel. The result is the formation of ghost keratin that may, in turn, induce dentinoid. The similarities between this lesion and the craniopharyngioma have previously been mentioned.
Treatment
These lesions are surgically removed and rarely recur after excision.
Odontogenic Myxoma
This is a benign infiltrative lesion that is clinically indistinguishable from ameloblastoma. It is found in tooth-bearing areas, and a slight predilection for the mandible exists. It generally appears in the early third to fourth decades of life as a slow-growing expansile lesion. If odontogenic myxoma is left untreated, it is invasive and destructive. It is derived from dental mesenchyme (papilla) or follicle.
Radiographic findings
The radiographic appearance of this lesion is not distinctive. It appears quite similar to ameloblastoma (eg, multilocular radiolucency), though some authors believe that the individual loculations are somewhat smaller in odontogenic myxoma (myxofibroma).
Histologic characteristics
A few stellate fibroblasts with copious amounts of hyaluronic acid, scant collagen fibrils, and no capsule describe the histologic appearance of this lesion. The hyaluronic acid component stains with Alcian blue, reminding one of the appearance of Wharton jelly. This lesion looks like developing pulp and may be confused with a developing third molar.
Treatment
As with ameloblastoma, this lesion is treated with block excision. Recurrences occur although with somewhat less frequency than with ameloblastoma.
Ameloblastic Fibroma
Ameloblastic fibroma is a true mixed tumor arising from a combination of 2 embryonic tissues. The epithelial component is able to induce mesenchyme but not to the extent of developing dental hard tissues. It is a relatively uncommon tumor of young people (aged 5-20 y); 75% of ameloblastic fibromas are found in the posterior mandible in the area of a developing tooth. It is benign and expansile, growing as a pushing front rather than invading surrounding tissues.
Radiographic findings
This lesion appears as a uniocular or bilocular radiolucency, most often in the posterior mandible. The radiographic appearance is identical to that of unicystic ameloblastoma, and both lesions should be differential diagnoses because they affect similar age groups and have similar clinical and radiographic appearances. Histologic examination differentiates the two.
Histologic characteristics
The epithelial component of this lesion is almost identical to that of ameloblastoma; however, the connective tissue component looks like dental pulp. It is a young, cellular, homogenous connective tissue without much dense collagen. The epithelial and connective tissue components grow together inside a capsule.
Treatment
The treatment of this lesion is block excision with a border of normal bone. With simple enucleation, recurrence rates of 20-40% have been reported. Sarcomatous change (ameloblastic fibrosarcoma) has also been reported with recurrence or inadequate excision.
Ameloblastic Fibro-odontoma
Ameloblastic fibro-odontoma is an extremely rare odontogenic lesion that develops dental hard tissues (eg, dentin, enamel, cementum). It appears most often before age 20 years and has a slight predilection for the premolar area in either jaw. Although these lesions can become quite large, they generally do not have much growth potential.
Radiographic findings
Ameloblastic fibro-odontoma appears as a well-demarcated radiolucency with a large central opacity. These lesions almost always are found in association with a tooth. Some similarity exists in radiographic appearance to that of the Pindborg tumor and Gorlin cyst because this is a mixed radiolucent/radiopaque lesion. If located in the anterior mandible, AOT also may be included in the radiographic differential diagnoses.
Histologic characteristics
This lesion has the histologic characteristics of ameloblastic fibroma. However, epithelial induction of connective tissue occurs to the point of histodifferentiation, leading to presence of dentin, enamel, and/or cementum in the microscopic presentation.
Treatment
Surgical excision of ameloblastic fibro-odontoma is the usual proposed treatment. These lesions do not often recur. The literature contains some support for sarcomatous change with recurrence.
Complex Odontoma
Complex odontoma lesions represent further histologic differentiation of the odontogenic pluripotential epithelium. Findings from this lesion resemble those of ameloblastic fibro-odontoma but extended one step further. The epithelium in this lesion has involuted, leaving disorganized dental hard tissues in place. These are common lesions, and they persist throughout life. They are usually detected in adolescence and have a predilection for the mandibular molar regions; however, they can be found in other areas of the jaws.
Radiographic findings
These lesions are generally described as sunburst radiopacities surrounded by a thin, uniform, radiolucent rim. Although this description may have some superficial resemblance to the radiographic description of osteosarcoma, the association with a tooth, the clear demarcation of the lesions' borders, and the lack of pain and/or swelling serve to delineate this very benign lesion from osteosarcoma.
Histologic characteristics
The histodifferentiation of this lesion is extended one step further than that of ameloblastic fibro-odontoma. In complex odontoma, a physiologic reduction of the ameloblastic epithelium is found. A mixed honeycomb presentation of enamel, cementum, dentin, and pulpal tissue is present. Histodifferentiation but no morphodifferentiation is observed in this lesion.
Treatment
Simple removal or radiographic observation is the method of treatment. These lesions do not recur.
Compound Odontoma
This is the most common odontogenic tumor. It represents the product of both histodifferentiation and morphodifferentiation of odontogenic tissues, resulting in what appears as a cluster of multiple abortive teeth. It is most commonly found in the maxillary anterior alveolar bone but may be located anywhere within the tooth-bearing segments of the jaws. It is often responsible for preventing normal tooth eruption, thus it is usually discovered during adolescence.
Radiographic findings
Multiple tiny toothlike structures are contained within a fine radiolucent rim.
Histologic characteristics
Histology of compound odontomas approaches normal tooth structure. Gross clinical examination is usually sufficient for diagnosis.
Treatment
Simple removal is the method of treatment. These lesions do not recur.
Cementoblastoma
Cementoblastoma, as distinguished from cementoma, is a true neoplasm of cementum. This benign neoplasm is rare and is usually observed in patients younger than 25 years. It is most often found in association with the apex of the mandibular first molars (50% of lesions), and it is never found in association with the anterior dentition. The lesion is usually asymptomatic, although occasionally the associated tooth may be slightly sensitive to percussion.
Radiographic findings
A round opaque sunburst mass attached to the apex of a tooth that is well-demarcated and surrounded by a thin radiolucent rim is observed. The lesion obscures the lamina dura. Students sometimes confuse it with condensing osteitis, a common lesion resulting from low-grade periapical irritation that stimulates bone growth. Although the most usual location for the 2 lesions is the same, condensing osteitis does not obscure the periodontal ligament (PDL) space and tends to be more irregular in outline. The mature cementoma, also known as periapical cemental dysplasia, is another common lesion that students may confuse with cementoblastoma. However, cementoma is usually located in the mandibular anterior region and does not obscure the PDL space. Cementomas actually have 3 developmental stages: osteolytic (at which point the lesion appears as a radiolucency), cementoblastic (mixed radiolucent/radiopaque), and mature (radiopaque).
Histologic characteristics
Plump cementoblasts separated by cemental partitions form the histology of this encapsulated lesion.
Treatment
Removal of attached tooth and tumor is the method of treatment. No recurrences are reported.
Multimedia
Keywords
mandibular cysts and odontogenic tumors, periapical cyst, radicular cyst, dentigerous cyst, primordial cyst, residual cyst, odontogenic mandibular cysts, lateral periodontal cyst, gingival cyst of the newborn, Bohn nodules, Epstein pearls, predeciduous dentition, gingival cyst of the adult, odontogenic keratocyst, OKC, basal cell nevus syndrome, nonodontogenic mandibular cysts, Stafne bone cyst, Stafne's bone cyst, static bone cavity, defect of the mandible, lingual mandibular bone cavity, static bone cyst, latent bone cyst, Stafne bone defect, Stafne's bone defect, traumatic bone cyst, solitary bone cyst, hemorrhagic cyst, extravasation cyst, unicameral bone cyst, simple bone cyst, idiopathic bone cavity, focal osteoporotic bone marrow defect
aneurysmal bone cyst, ameloblastoma, adenomatoid odontogenic tumor, AOT, calcifying epithelial odontogenic tumor, CEOT, Pindborg tumor, keratinizing and calcifying odontogenic cyst, KCOC, Gorlin cyst, odontogenic myxoma, myxofibroma, ameloblastic fibroma, ameloblastic fibro-odontoma, complex odontoma, compound odontoma, cementoblastoma, mandibular cysts, odontogenic tumors





Good post..thanx fr the valuable in formation..y don't you read the case report on CEOT?and gather more knowledge..here : http://dentistryandmedicine.blogspot.com/2010/12/calcifying-epithelial-odontogenic.html
Trả lờiXóaFacial surgery is well effective and better in treat disease easily and fast. That make good attraction of people which want it. Sound increase its better and effective for good result.
Trả lờiXóafacial surgery
Trả lờiXóaPlacidway offers very good access to doctors and prices to match anyone:
Dentures in Mexico
I was diagnose with genital warts since 2012 i have be taking lot treatment and all i got is outbreak. in 2015 I gave up the treatment because I can't continues wasting time and money on treatment at the end it will not cure me. about 6 weeks ago i did natural research online I had So many people talking good about natural remedy, after the research i was recommended to Dr onokun, And I wrote to him through his email and told him my problem after some conversations with him he gave me natural treatment after 1 week Dr onokun treated me i got cured permanently. and i went to see my doc he confirmed that the diseases has gone out from my body. every patients should know there is 100% natural hpv cure. contact Dr onokun his email address: dronokunherbalcure@gmail.com
Trả lờiXóa