Introduction
Surgical practice begins with a detailed knowledge of anatomy. While the anatomy of the orbit has not changed over time, advances in surgical procedures have challenged surgeons to apply a detailed understanding of the anatomic relationships of the orbit. This article addresses orbital anatomy with emphasis on procedures and clinical applications in otolaryngology and head and neck surgery. Discussion of eyelid anatomy is reserved for other eMedicine articles (see Eyelid Anatomy).
Osteology
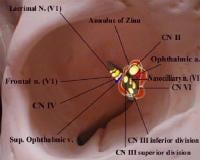
The orbit functions to protect, support, and maximize function of the eye. The orbit is shaped as a quadrilateral pyramid with its base in plane with the orbital rim. Seven bones conjoin to form the orbital structure. The orbital process of the frontal bone and the lesser wing of the sphenoid form the orbital roof. The orbital plate of the maxilla joins the orbital plate of the zygoma and the orbital plate of the palatine bones to form the floor. Medially, the orbital wall consists of the frontal process of the maxilla, the lacrimal bone, the sphenoid, and the thin lamina papyracea of the ethmoid. The lateral wall is formed by the lesser and greater wings of the sphenoid and the zygoma (see Image 1).
The orbits are aligned so that the medial walls are parallel and the lateral walls are perpendicular. The arc from medial to lateral wall in each orbit is 45°. Lines dropped through a central anterior-to-posterior axis of each orbit bisect at a 45° angle. The floor is two-thirds the depth of the orbit. The average dimensions of the orbit are as follows:
- Height of orbital margin - 40 mm
- Width of orbital margin - 35 mm
- Depth of orbit - 40-50 mm
- Interorbital distance - 25 mm
- Volume of orbit - 30 cm3
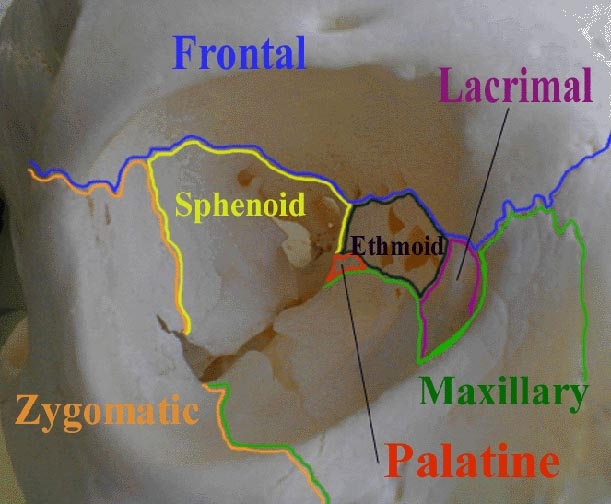
The superficial bony orbit is defined by the orbital margin, which is rectangular with rounded corners. The margin is discontinuous at the lacrimal fossa. The supraorbital notch is within the supraorbital rim and is closed to form the supraorbital foramen in 25% of individuals. The supratrochlear notch is medial to the supraorbital notch. The trochlea is a cartilaginous ring that supports the superior oblique muscle. The trochlea attaches to the periorbita within the fovea trochlearis along the superior-medial orbit. The infraorbital foramen is located 10 mm inferior to the zygomaxillary suture. Laterally, the orbital rim is marked by the Whitnall tubercle, which is 10 mm inferior to the zygomaticofrontal suture. The tubercle is the site of attachment of the lateral canthal tendon (see Image 2).
The major nerves and vessels to the orbit and globe enter through 3 openings. The superior orbital fissure is bounded by the lesser and greater wings of the sphenoid. The greater wing of the sphenoid, the maxilla, and the palatine bones of the orbit form the boundaries of the infraorbital fissure. The optic canal is at the apex of the orbit and lies within the sphenoid bone. The orbital fissures and canals with corresponding structures are as follows:
- Superior orbital fissure
- Cranial nerves (CN) III, IV, and VI
- Lacrimal nerve
- Frontal nerve
- Nasociliary nerve
- Orbital branch of middle meningeal artery
- Recurrent branch of lacrimal artery
- Superior orbital vein
- Superior ophthalmic vein
- Inferior orbital fissure
- Infraorbital nerve
- Zygomatic nerve
- Parasympathetics to lacrimal gland
- Infraorbital artery
- Infraorbital vein
- Inferior ophthalmic vein branch to pterygoid plexus
- Optic canal
- Optic nerve
- Ophthalmic artery
- Central retinal vein
The anterior and posterior ethmoid foramina lie in the medial wall of the orbit along the frontoethmoidal suture line. The anterior and posterior ethmoid arteries pass through these foramina and are important surgical landmarks. The arteries mark the level of the cribriform plate and the relationship of the anterior cranial fossa to the orbits. The ethmoid arteries mark the superior limit for osteotomies during medial maxillectomy. The distance from the orbital rim to the anterior ethmoid artery is approximately 20-25 mm. The distance between the anterior and posterior ethmoid arteries averages 12 mm, with a range of 8-19 mm. The optic ring averages 6 mm from the posterior ethmoid artery, with a range of 5-11 mm. Knowledge of these distances safely guides the surgeon along the medial orbital wall.
The infraorbital sulcus crosses the floor of the orbit and carries the infraorbital artery, infraorbital vein, and infraorbital nerve from the infraorbital fissure to the infraorbital foramen. Clinically, the infraorbital foramen provides a route of spread for infection or maxillary tumors to the orbit and the skull base. The surgeon must avoid injury to the infraorbital neurovascular bundle when performing a midface degloving approach.
Lacrimal System
The lacrimal system produces, distributes, and drains tears. Tears are produced by the lacrimal gland and multiple accessory glands. The lacrimal gland is divided into the orbital lobe and the palpebral lobe by the lateral horn of the levator aponeurosis. The lacrimal gland is oriented in the superior-temporal region of the orbit and lies in the fossa glandular lacrimalis. The palpebral lobe can be seen by everting the upper lid where it extends to within a few millimeters of the tarsus. The ducts of the orbital lobe traverse the palpebral lobe before opening into the fornix.
The gland can be recognized by its pink-gray color and glandular surface. Although the gland appears to have a capsule, this is really a combination of surrounding connective tissue insertions. The lacrimal nerve, a branch of the ophthalmic division of CN V, provides sensory innervation to the lacrimal gland.
Tears are drained via a conduit of tubes along the medial angle of the eye. The system is composed of paired lacrimal papillae, puncta, and canaliculi that connect to form the common canaliculus, lacrimal sac, and nasolacrimal duct. The common canaliculus inserts into the lacrimal sac at an angle to produce the valve of Rosenmüller. This valve prevents reflux of tears into the canalicular system. The tears are stored in the lacrimal sac and then drain through the nasolacrimal duct that opens into the inferior meatus of the nasal cavity. The nasolacrimal duct is just anterior and lateral to the uncinate process and can be injured in endoscopic sinus surgery.
Connective Tissue Planes
The contents of the orbit are separated and supported by multiple connective tissue planes. The detailed anatomy of these connective tissue structures is complicated and beyond the scope of this article. In general, the connective tissue boundaries can be divided into 4 main units as follows:
- The bulbar fascia (ie, Tenon fascia) surrounds and protects the globe posteriorly from the limbus. The extraocular muscles penetrate the bulbar fascia to insert on the globe. The fascia provides a barrier between the globe and the retrobulbar fat, allowing free motion of the globe.
- Multiple connective tissue septa extend from the globe to the periorbita like spokes on a wheel. These septa are located 360° around the globe and function to stabilize the globe centrally within the orbit. The septa have enough laxity to allow free movement of the globe.
- Each extraocular muscle has an individual connective tissue sheath. As the sheaths progress anteriorly toward the globe, they fuse to form a confluent muscle sheath. Connective tissue struts extend medially and laterally from the respective muscle sheaths to form the medial and lateral check ligaments.
- The orbital structures are contained within the periosteal lining of the orbit, which can be elevated in surgery to expose the bony orbit. By keeping the periosteum intact, the surgeon can work in the anterior orbit without injuring the orbital contents.
Extraocular Muscles
Each orbit contains 6 extraocular muscles that function together to move the eye: 4 rectus muscles (ie, superior, inferior, lateral, medial) and 2 oblique muscles (ie, superior, inferior). The levator palpebrae muscle functions to elevate the upper lid. The actions of each extraocular muscle are as follows:
- Medial rectus - Adduction
- Lateral rectus - Abduction
- Superior rectus - Elevation, adduction, intorsion
- Inferior rectus - Depression, adduction, extorsion
- Inferior oblique - Extorsion, elevation, abduction
- Superior oblique - Intorsion, depression, abduction
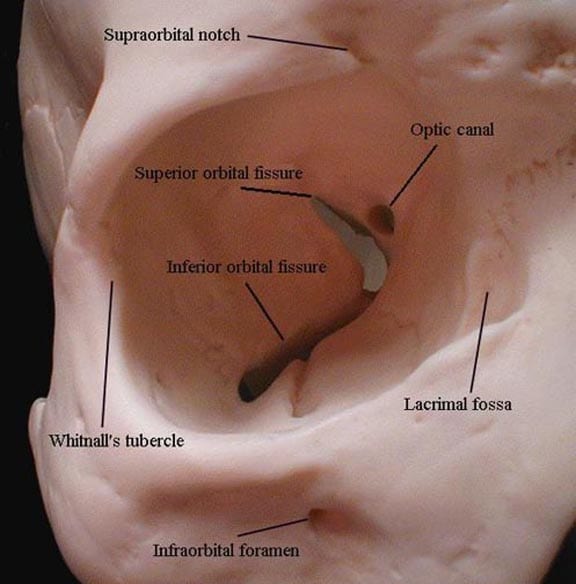
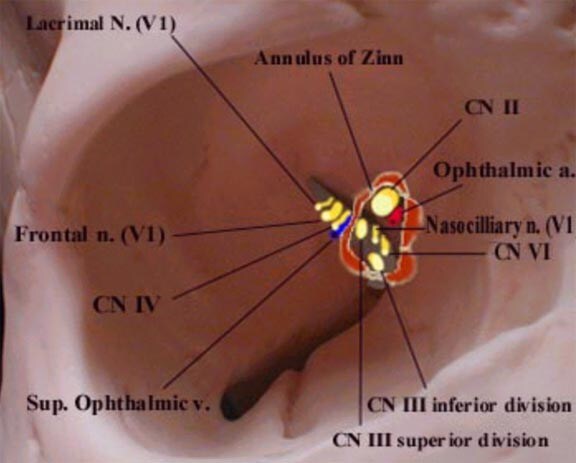
The rectus muscles originate at the annulus of Zinn, a fibrous tendon that encircles the optic foramen (see Image 3). The annulus of Zinn is divided into the superior Lockwood tendon and the inferior tendon of Zinn. The annulus is continuous with the dura of the middle cranial fossa. The superior and medial rectus muscle sheaths are adherent to the optic nerve sheath at the annulus.
Unlike the rectus muscles, the superior and inferior oblique muscles originate separately from the posterior orbital wall. The extraocular muscles attach to the sclera anterior to the equator of the eye. The superior oblique first passes through the trochlea and then redirects in a posterior-lateral direction to attach to the eye. The trochlea is a cartilaginous saddle with dense fibrous condensations that attach to the periosteum of the orbit.
Multiple medical conditions can cause hypertrophy of the extraocular muscles with clinical presentation of proptosis, diplopia, and orbital pain. Trokel and Hilal showed that exophthalmos of Graves disease was the most common cause of extraocular muscle hypertrophy.1 Graves disease was the cause in 65.6% of cases, while carotid cavernous fistula caused 17.1%, pseudotumor caused 10%, and orbital tumor caused 7.1% of cases of extraocular muscle hypertrophy.
Malignant exophthalmos is most commonly associated with Graves disease, but it can be caused by other endocrine disorders. Graves ophthalmopathy has been linked to thyroid-stimulating hormone and a factor that causes increased deposition of mucopolysaccharides into orbital fat. Exophthalmos can lead to corneal abrasion, chemosis, ophthalmoplegia, and retinal venous congestion. Several procedures have been developed that involve removing a portion of the bony orbit to decompress the orbital contents.
Innervation of the Orbit
The innervation of the orbit can be divided into 4 functional components: general somatic efferent (extraocular muscles), general somatic afferent (sensory), general visceral efferent (autonomic), and special sensory afferent (vision). The general somatic efferents include the motor division of the oculomotor nerve (CN III), the trochlear nerve (CN IV), and the abducens nerve (CN VI).
The oculomotor nerve (CN III) pierces the dura at the lateral posterior clinoid process, courses through the lateral aspect of the cavernous sinus, and enters the inferior portion of the supraorbital fissure. Within the cavernous sinus, the nerve divides into superior and inferior branches. The superior branch supplies the superior rectus muscle and the levator palpebrae superioris, while the inferior branch passes through the annulus of Zinn to supply the medial rectus, inferior rectus, and inferior oblique. The inferior branch also carries preganglionic parasympathetic fibers to the ciliary ganglion.
The trochlear nerve (CN IV) travels through the cavernous sinus and enters the orbit through the superior orbital fissure outside of the annulus of Zinn. The trochlear nerve innervates the superior oblique muscle. The abducens nerve (CN VI) has a long tortuous intracranial course. The nerve passes along the clivus and through the inferior petrosal sinus at the junction of the petrous portion of the temporal bone and occipital bone. The nerve bends over the petrous ridge and passes inferior to the petroclinoid ligament. It then travels through the Dorello canal lateral to the carotid artery and medial to the trigeminal ganglion. The abducens nerve enters the orbit through the superior orbital fissure within the annulus of Zinn and innervates the lateral rectus. The relatively long intracranial course of the abducens nerve makes it susceptible to injury secondary to trauma, tumor, aneurysm, and infection.
The trigeminal nerve supplies general sensory innervation to the orbit and surrounding structures. The trigeminal nerve originates at the lateral and ventral portion of the pons. The nerve enters the Meckel cave, which is formed by a split in the dura along the petrous temporal bone in the middle cranial fossa. The trigeminal ganglion rests in the Meckel cave posterior and lateral to the cavernous sinus and the internal carotid artery. The ophthalmic branch extends from the trigeminal ganglion and passes through the cavernous sinus to the orbit via the superior orbital fissure.
Within the orbit, the ophthalmic nerve branches into the lacrimal, frontal, and nasociliary nerves. The lacrimal nerve innervates the lacrimal gland and accepts postganglionic parasympathetic fibers. The parasympathetic fibers travel from the lacrimal nucleus in the pons via the nervus intermedius to the greater superficial petrosal nerve, to the vidian nerve, to the sphenopalatine ganglion, to the zygomatic branch of the maxillary nerve, to the zygomaticotemporal nerve, to the lacrimal nerve to innervate the lacrimal gland.
The frontal branch splits to form the supraorbital and supratrochlear nerves that exit the orbit at the superior orbital rim and innervate the eyebrow and scalp. The nasociliary branch enters the orbit through the annulus of Zinn and then gives off short and long ciliary nerves to the globe. The long ciliary nerves carry sympathetics from the superior cervical ganglion responsible for dilatation of the pupil. The short ciliary nerves pass through the ciliary ganglion and do not synapse. A branch of the nasociliary nerve runs along the medial orbital wall and gives off the posterior and anterior ethmoid nerves, which innervate the mucosal lining of the ethmoid sinuses and part of the nasal cavity. The infratrochlear nerve is also a branch of the nasociliary nerve and provides sensory innervation to the medial lower lid, side of nose, conjunctiva, and lacrimal sac.
The maxillary division of the trigeminal nerve leaves the middle cranial fossa through the foramen rotundum and enters the pterygopalatine fossa. Within the fossa, it branches into purely sensory infraorbital, zygomatic, and posterior superior alveolar nerves. The infraorbital nerve travels along the infraorbital sulcus and exits the infraorbital foramen. The zygomatic nerve divides into the temporal and facial branches. The posterior superior alveolar nerve primarily innervates the teeth.
The optic nerve extends from the optic chiasm to enter the orbit through the optic canal. The intraorbital portion of the optic nerve is 30 mm in length and 4 mm in diameter. The optic nerve is covered by dura, arachnoid, and pia from the sclera to the canal, where the dura is continuous with the periosteum of the orbit.
The surgeon must be aware of the oculocardiac reflex when manipulating the contents of the orbit. The reflex arc can cause bradycardia, hypotension, and nausea when pressure is applied to the globe or when the extraocular muscles are stretched. The reflex is triggered by afferent fibers of the trigeminal nerve, which synapse with visceral motor nucleus neurons of the vagal nerve in the reticular formation of the brain stem. When applying pressure to the globe during surgery, notify the anesthesiologist of potential changes in the patient's hemodynamic status.
Vascular Supply of the Orbit
An anastomosing network of vessels derived from the internal and external carotid artery systems supplies the orbit. The major arterial supply to the orbit is the ophthalmic artery, the first major branch of the internal carotid artery. The ophthalmic artery originates from the internal carotid as it exits the cavernous sinus. The ophthalmic artery courses on the inferior aspect of the optic nerve and enters the orbit through the optic canal. The artery gives off many branches with a significant amount of variability. In general, the branches of the ophthalmic artery can be divided into 3 groups of vessels (ie, ocular, orbital, extraorbital) based on their target organs.
The ocular branches include the central retinal artery, ciliary arteries, and collateral branches to the optic nerve. The orbital branches are the lacrimal artery, muscular arteries, and periosteal branches. Extraorbital branches include the posterior and anterior ethmoid arteries, supraorbital artery, medial palpebral artery, dorsal nasal artery, and supratrochlear artery.
The orbital and extraorbital vessels further divide into branches that anastomose with vessels from the external carotid artery system. The zygomatic artery derives from the lacrimal artery and then branches into temporal and facial divisions that anastomose with branches of the superficial temporal artery. The lacrimal artery has a branch to the gland and a recurrent meningeal branch, which returns to the middle cranial fossa. The lateral palpebral artery branches from the lacrimal artery to supply a cascade of vessels in the eyelid and anastomose with the medial palpebral artery. The medial palpebral artery is supplied by a combination of the dorsal nasal artery and the angular artery, which comes from the external carotid system.
The posterior and anterior ethmoid arteries pass through their respective foramina in the frontal bone. The anterior ethmoid artery is the larger of the 2 arteries and supplies the anterior and middle ethmoid air cells, the frontal sinus, and the dura of the anterior cranial fossa via a meningeal branch. The supraorbital artery supplies the muscles of the eyebrow and forehead and has connection with the frontal branch of the superficial temporal artery. The supratrochlear artery terminates in the scalp and is the artery upon which paramedian forehead flaps for nasal reconstruction are based.
The infraorbital artery is a branch of the external carotid system via the internal maxillary artery. The infraorbital artery branches from the internal maxillary artery in the pterygopalatine fossa and enters the orbit through the infraorbital fissure to travel across the floor of the orbit in the infraorbital sulcus. The infraorbital artery exits the skull at the infraorbital foramen and forms a network with vessels of the facial artery and zygomatic artery.
Venous drainage of the orbit occurs through 2 major veins, the superior and inferior ophthalmic veins. Venous drainage of the orbit, like its arterial supply, occurs through an anastomosing network of internal and external systems. The orbital veins are valveless; therefore, direction of venous drainage depends on pressure gradients.
The superior ophthalmic vein collects flow from the ethmoidal, ciliary, lacrimal, and superior vortex tributaries. The vein passes through the superior orbital fissure and drains into the cavernous sinus. The inferior ophthalmic vein is supplied by a diffuse plexus of veins in the floor of the orbit. The inferior ophthalmic vein empties into the superior ophthalmic vein within the orbit and has a small branch, which drains into the pterygoid venous plexus. The central retinal vein empties directly into the cavernous sinus. The veins of the external orbit drain into the angular vein of the face that has connections with the superior ophthalmic vein system.
The dual arterial supply and valveless venous system provide the orbit with a rich vascular supply. In obstruction of the internal carotid system, collateral flow from the external carotid system can provide adequate flow to the orbit. The veins allow flow to reverse in case of obstruction.
The anastomosing network of vessels can contribute to clinical problems. A carotid cavernous sinus fistula can develop secondary to head trauma or iatrogenic injury, or it can occur spontaneously. The anatomic abnormality consists of a communication between the internal carotid artery and the venous plexus of the cavernous sinus. Carotid cavernous sinus fistula presents with pulsatile exophthalmos, bruit, chemosis, engorgement of epibulbar veins, increased intraocular pressure, ocular ischemia, and visual loss. The diagnosis is confirmed by visualizing the fistula with angiography. In cases of severe orbital infection, the valveless venous system allows spread of infected emboli to the cavernous sinus and can cause cavernous sinus thrombosis.
Conclusion
The anatomy of the orbit has many significant applications in otolaryngology and head and neck surgery. Understanding these important anatomic relationships enables surgeons to perform procedures safely. Knowledge of these concepts helps surgeons recognize problems and complications when they occur.
Multimedia
 | Media file 1: This image of the right orbit shows the 7 bones that contribute to its structure. |
 | Media file 2: This image of the right orbit shows superficial landmarks, optic canal, and superior and inferior orbital fissures. |
 | Media file 3: Diagram of right orbit that shows the relationship of entering nerves and vessels to the annulus of Zinn. |
Keywords
orbit anatomy, eye anatomy, orbital anatomy, orbital roof, orbital floor, supraorbital rim, trochlea, supratrochlear notch, infraorbital foramen, optic canal, optic nerve, lacrimal system, bulbar fascia, extraocular muscles, oculomotor nerve, trochlear nerve, trigeminal nerve, oculocardiac reflex, ophthalmic artery, infraorbital artery



Không có nhận xét nào:
Đăng nhận xét