Introduction
Knowledge of the anatomy of the mandible and the muscular forces applied to it is the key to proper reduction of mandibular fractures. The goal in reduction is to restore premorbid occlusion, allowing patients to resume masticatory functions. Prior to repair, patients must be thoroughly evaluated.
As with any trauma, the fundamentals of good trauma care must be followed. The airway must be secured, and breathing and circulation must be confirmed. Possible cervical spine (C-spine) injury needs to be ruled out. With mandibular fractures, earlier reduction is associated with better outcomes. Although, if other injuries dictate, repair may be delayed 5-7 days, surgical correction is recommended as soon as possible. Current concepts include early intervention with wide surgical exposure to allow for precise alignment and rigid fixation.
For excellent patient education resources, visit eMedicine's Back, Ribs, Neck, and Head Center, Breaks, Fractures, and Dislocations Center, and Teeth and Mouth Center. Also, see eMedicine's patient education articles Broken Jaw and Broken or Knocked-out Teeth.
History of the Procedure
The first descriptions of treating mandible fractures date back to Egypt around 1650 BC. Hippocrates talked of reapproximation and immobilization. Proper occlusion was first addressed in 1180 in Salerno, Italy. Fixation of the maxilla to the mandible was first used in 1492. In the 1950s, the Arbeitsgemeinschaft für osteosynthesefragen/Association for the Study of Internal Fixation (AO/ASIF) was founded. Early AO plates were stainless steel. Other materials included cobalt-chromium and titanium. Most internal fixation systems use titanium or a titanium alloy. Currently, resorbable plates are being investigated.
Early techniques used to immobilize mandible fractures included bandage immobilization and intermaxillary fixation. During World War II, realignment with open access and wire fixation was popular. More recently, a tremendous amount of fracture management with rigid plate fixation has occurred. Plates were made to span and stabilize the fracture. Plates were then developed to be either compression or noncompression. Furthermore, the compression plates could be made to compress the fracture in an eccentric manner. Compression is achieved by inclines built into the plate. When the screws adjacent to the fracture are activated, the fracture segments are forced together, resulting in primary bone healing. These forces can be directed at the inferior compression site of the mandible or superiorly to the tension aspect of the mandible.
Champy describes using a noncompression, monocortical plate in the region of the external oblique ridge. Ellis has had excellent clinical results using this technique for angle fractures of the mandible.1
Current management consists of early surgical intervention with wide exposure of the fracture and placement of rigid fixation.
Problem
When an external force is imposed on the mandible that is strong enough to cause the mandible to fracture, the surgeon must anticipate associated injuries. Although a single blow to the mandible can yield an isolated fracture, more commonly, 2 sites are involved. The surgeon should always be wary if only one fracture site is identified. For example, trauma to the side usually yields an ipsilateral body fracture and a contralateral subcondylar fracture. A classic severe blow to the symphysis produces a symphyseal fracture and bilateral subcondylar fractures. With bilateral fractures, parasymphyseal or body, always protect the airway from obstruction by the retrodisplaced tongue. In a motor vehicle accident or a gunshot wound, multiple fractures should be suspected along with injuries to the soft tissue, C-spine, and central nervous system. These concomitant injuries are seen in as many as 30% of facial trauma cases.
These injuries may be life threatening and should be dealt with as a high priority. As in all patients with traumatic injuries, the airway should be secured, the patient should be breathing, and the circulation should be stable. The C-spine should always be assessed radiologically and clinically, and injuries here should be ruled out prior to manipulation of the neck. Some C-spine injuries can be asymptomatic. Appropriate consultations should be made to assess the patient. The secondary survey can then be performed, including a full head and neck examination.
Airway compromise often accompanies mandible fracture. Causes can include intraoral bleeding, edema, loose teeth or dentures, and posterior displacement of the mandible and/or tongue due to a flailed segment of the mandible. Consider an emergent tracheotomy or a cricothyrotomy when an obstruction persists despite use of basic cardiopulmonary resuscitation (CPR).
Treatment goals are to restore function and premorbid occlusion. Mastication, speech, and normal range of oral motion should be achieved. Contour defects must be corrected. Early treatment curtails the possibility of infection.
Frequency
The areas of the mandible most commonly fractured include the condylar-subcondylar region, body, and angle. Location of the fractures and associated frequency are as follows:
- Condyle - 29%
- Angle - 24%
- Symphysis - 22%
- Body - 16%
- Ramus - 1.7%
- Coronoid - 1.3%
The types of fractures commonly seen due to motor vehicular accident have decreased significantly with the use of restraint devices. The symphyseal and bilateral parasymphyseal fractures caused by the mandible striking the steering wheel or dashboard are rarely seen in patients using a seat belt.
The average number of mandibular fractures per patient is 1.5-1.8. Ten percent of patients have more than 2 fractures.
Because of the inherent design of the mandible, a unilateral fracture is rare. Children younger than 6 years make up only 1% of the total number of cases. Of note, children with mandibular fractures often have other associated injuries.
Etiology
With increased use of vehicular restraints, the incidence of maxillofacial trauma resulting from motor vehicle accidents has been on the decline. On the other hand, the number of mandibular fractures resulting from assault has risen. Other causes include injury from a fall, sports-related injuries, and bicycle accidents. Causes are summarized as follows:
- Vehicular accidents - 43%
- Assaults - 34%
- Work related - 7%
- Fall - 7%
- Sporting accidents - 4%
- Miscellaneous - %5
Presentation
History can help in the diagnosis. Underlying bone disorders and previous mandibular trauma may predispose a patient to traumatic fractures. The type and direction of force are important, as is the object causing the fracture. Symptoms often described include pain, trismus, difficulty chewing, and anesthesia or paresthesia of the lower lip and chin.
On examination, findings include abnormal mandibular movements, malocclusion, change in facial contour and mandibular arch form, tenderness, swelling, redness, lacerations, hematoma, and ecchymosis. Loose and fractured teeth should be evaluated and counted. If teeth are missing, consider a chest radiograph to rule out aspiration.
Premorbid occlusion can be confirmed by examining the wear facets on the surfaces of the opposing teeth. Patients are quite sensitive to changes in their occlusion and can appreciate displacements smaller than 1 mm. It must be remembered that not all patients have ideal occlusion (ie, only 74% of the population have an angle class I bite). The remainder has either retrognathia (angle class II, 24%) or prognathia (angle class III, 1%).
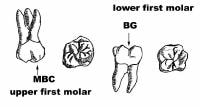
Angle classification is based on the relationship of the mesial-buccal cusp of the maxillary first molar to the buccal groove of the mandibular first molar. (Mesial is anterior in reference to the sagittal plane and distal is posterior to that same plane.) Anatomy is shown in the image below.
Oral and maxillofacial surgeons also use the relationship of the canine teeth to determine the occlusal class. Class I occlusion refers to the mesial-buccal cusp of the maxillary first molar's contact with the mandibular first molar's buccal groove. The mesial-buccal cusp lies in front of (or mesial to) the groove in class II occlusion. In angle class III occlusion, the mesial-buccal cusp of the maxillary first molar falls behind (or distal to) the groove.
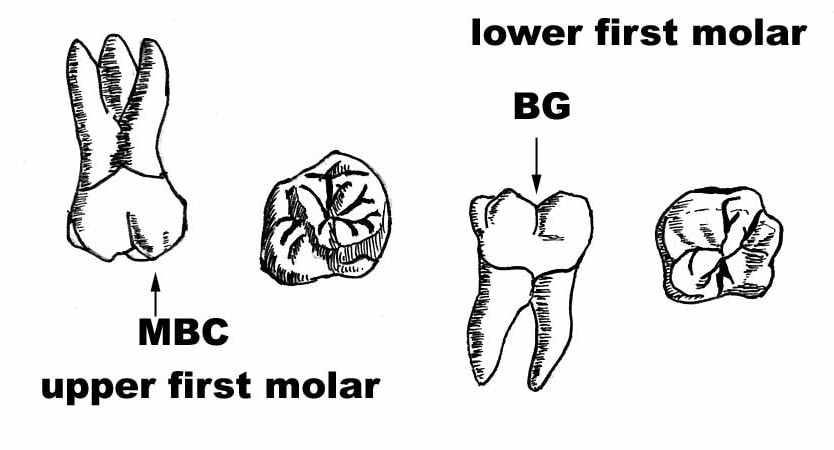
Fractures that occur in the region of the teeth are considered to be compound fractures, which can be predisposed to bacterial contamination from the oral cavity. An open laceration and bleeding from the site also may be evident with compound fractures. These types of fractures should, therefore, be prophylactically treated with antibiotics. If the mucosa has not been violated, then clinical findings can be limited to ecchymosis. If the third division of the trigeminal nerve (the inferior alveolar or mental nerve) has been injured, the patient may have paresthesia or anesthesia of the chin. Documenting this and the function of the marginal mandibular nerve (branch of cranial nerve VII) is important prior to surgical intervention. The nerve course is shown in the image below.
Spasm of the muscles of mastication due to trauma can result in trismus, limiting a proper oral examination. Facial edema, erythema, and pain are also associated with mandibular fractures. Bilateral parasymphyseal/body and, at times, subcondylar fractures can result in the posterior displacement of the tongue, leading to airway compromise. In accordance with the tenets of trauma care, the airway should always be addressed first.
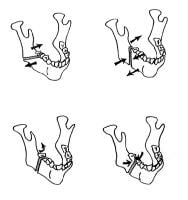
The fracture may be classified as simple, greenstick, compound, comminuted, or pathologic. Furthermore, classification can take into account forces influenced by muscular distraction. Muscular force can act favorably (nondisplaced fracture) or unfavorably (displaced fracture). Displacement can occur in either the horizontal or the vertical plane. Favorable and unfavorable fractures are shown below.
Indications
Generally, some form of therapy is needed for a fracture of the mandible. Perform the most conservative treatment that allows for reduction of the fracture while preserving the premorbid occlusion.
Observation
Historically, for minimally displaced fractures that were of a favorable type, a Barton-type head bandage gave enough support for the fracture to heal. This was especially true in children. A liquid or pureed diet was maintained for 4 weeks. The trends currently advocate early surgical intervention, wide access to the fracture site, and complete immobilization with rigid fixation.
Factors affecting fragment displacement include the direction and intensity of the traumatic force, direction and bevel of the fracture line, presence or absence of teeth in the fragments, direction of muscle pull, and extent of soft-tissue injury. In a favorable fracture, the muscle pull promotes splinting of the segments; muscle pull distracts the segments in an unfavorable fracture.
Muscles involved in opening the mouth include the anterior belly of the digastric muscle and the mylohyoid, geniohyoid, and genioglossus muscles. Oral closure is provided by the action of the temporalis, masseter, and the internal (or medial) pterygoid muscles. The only protrusion from the mandible is the external, or lateral, pterygoid muscle. The forces of these muscle groups, along with the bevel and angle of the fracture, determine whether or not a fracture is favorable or unfavorable.
Maxillomandibular fixation and closed reduction
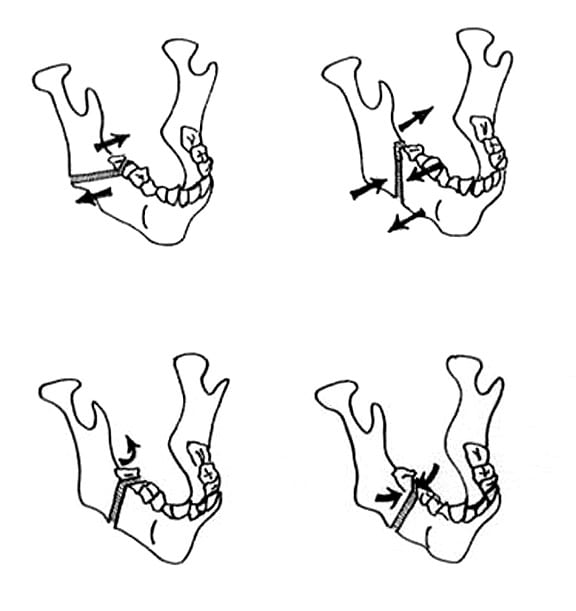
If external dressings are not sufficient, closed reduction can be accomplished with maxillomandibular fixation (MMF), formerly known as intermaxillary fixation (IMF; shown in the image below).
Cawood has described many ill effects of MMF when arch bars and ligatures are used. To avoid these types of issues, 4-point MMF can be used, as depicted in the image below. Otherwise, arch bars are placed with wire ligature (24-26 gauge) or composite resin.
Open reduction
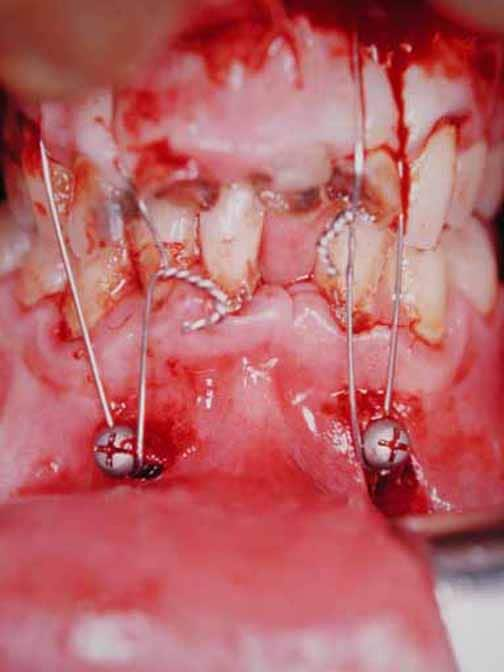
Open reduction is an excellent modality for fracture segment reduction. After MMF, an incision is made to allow for direct alignment of the segments. Access can be achieved via either an intraoral or extraoral incision, depicted below. To maintain fixation, titanium plates and screws or stainless steel wire may be used. Even with an incision, percutaneous access may be needed for the placement of plates, screws, or wire.
External fixation, shown in the image below, was popular in World War II but currently is not often employed. Principle indications are sites that have been infected or pathological fractures. It can also be used in edentulous patients with unstable fractures. Stainless steel pins and composite resin placed lateral to the mandible keep the fracture rigidly reduced.
Other alternatives include use of the patient's dentures to reduce the fracture. The dentures act as a splint, and with the use of circumferential mandibular wires, they can stabilize the fracture, as shown below. The upper and lower dentures can be wired together to maintain MMF. If the patient is edentulous but without dentures, a Gunning-type splint can be fabricated and used in the same manner as dentures.








Không có nhận xét nào:
Đăng nhận xét